Sunday Poster Session
Category: IBD
P0958 - Serum Protein Capillary Electrophoresis as a Biomarker for Endoscopic Disease Activity in Inflammatory Bowel Disease: A Prospective Pilot Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Jared Sninsky, MD, MSCR
Baylor College of Medicine / Michael E. DeBakey Veterans Affairs Medical Center
Houston, TX
Presenting Author(s)
Award: Presidential Poster Award
Jared Sninsky, MD, MSCR1, Ana-Maria Staicu, PhD2, Rongrong Huang, PhD3, Adith Ram, BA3, Jason K. Hou, MD, MS, FACG1
1Baylor College of Medicine / Michael E. DeBakey Veterans Affairs Medical Center, Houston, TX; 2North Carolina State University, Raleigh, NC; 3Baylor College of Medicine, Houston, TX
Introduction: Management of IBD has transitioned to a treat-to-target paradigm, aiming for defined objective treatment outcomes. C-reactive protein (CRP) has low sensitivity, while stool collection for fecal calprotectin faces challenges with patient adherence. There is a need for more accurate, accessible, and cost-effective blood-based biomarkers in IBD to optimize treat-to-target care.
Methods: We conducted a prospective pilot observational study of IBD patients, including both Crohn’s disease (CD) and Ulcerative Colitis (UC) patients, undergoing endoscopic evaluation for disease activity assessment. Serum protein capillary electrophoresis (SPEP) and C-reactive protein (CRP) were measured pre-procedure before colonoscopy. Wilcoxon rank-sum testing was used to compare SPEP components in g/dL (albumin, alpha-1, alpha-2, beta-1, beta-2, gamma) between patients with endoscopically active disease (eMayo> 1, SES-CD> 2) and those in remission. Logistic regression models were performed to determine discriminatory ability of SPEP components compared to CRP alone.
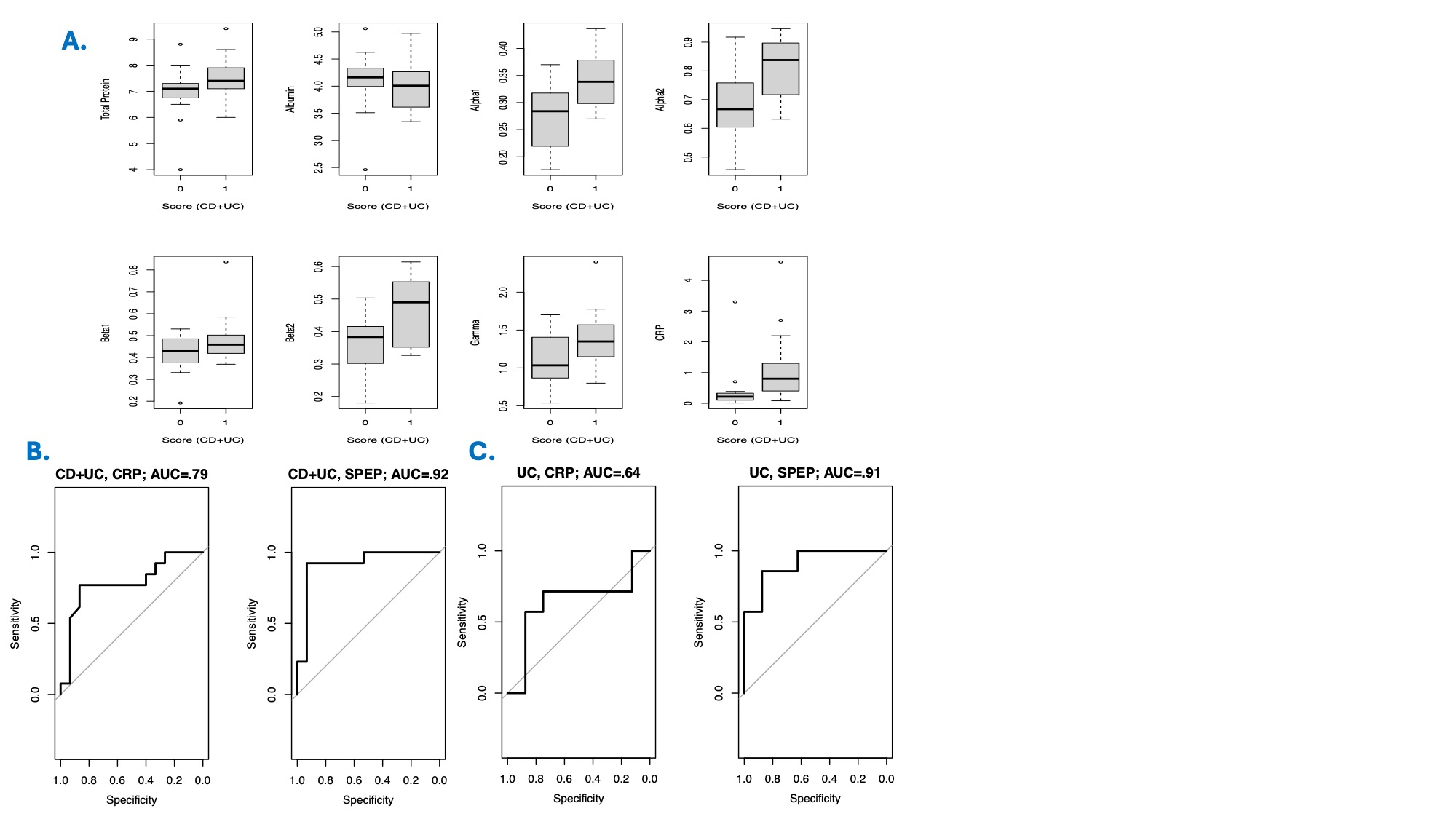
Results: Our pilot study included 28 patients with complete SPEP, CRP, and endoscopic data: 15 patients with UC and 13 patients with CD. The patient population was predominantly female (71%), White (68%), and non-Hispanic (82%), with an average age of 44 years (SD 16). Among all IBD patients, 46% had endoscopically active disease. In all IBD patients, significant elevations were observed in alpha-1 (95% CI: 0.01-0.12, p=0.009), alpha-2 (95% CI: 0.02-0.24, p=0.03), beta-2 (95% CI: 0.04-0.18, p=0.02), and CRP (95% CI: 0.10-1.0, p=0.01) levels among patients with active endoscopic inflammation (Fig 1A). In all IBD patients, a logistic regression model of CRP had an AUC of 0.79 compared to 0.89 for SPEP components (albumin, alpha-1, alpha-2, beta-1, beta-2, gamma) (Fig 1B). In CD patients, the AUC for CRP was 0.93 and 1.0 for SPEP components; while in UC patients, the AUC for CRP was 0.64 and 0.91 for SPEP components (Fig 1C).
Discussion: Several SPEP components are significantly upregulated in association with endoscopic inflammation in IBD, demonstrating superior discriminatory ability compared to CRP alone. Despite potential overfitting in this limited dataset without an independent testing cohort, SPEP components show clear promise in differentiating endoscopically active IBD. Our goal is to develop a model that integrates both CRP and SPEP components to create an accessible and accurate treat-to-target biomarker for inflammation in IBD.
Disclosures:
Jared Sninsky, MD, MSCR1, Ana-Maria Staicu, PhD2, Rongrong Huang, PhD3, Adith Ram, BA3, Jason K. Hou, MD, MS, FACG1. P0958 - Serum Protein Capillary Electrophoresis as a Biomarker for Endoscopic Disease Activity in Inflammatory Bowel Disease: A Prospective Pilot Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Jared Sninsky, MD, MSCR1, Ana-Maria Staicu, PhD2, Rongrong Huang, PhD3, Adith Ram, BA3, Jason K. Hou, MD, MS, FACG1
1Baylor College of Medicine / Michael E. DeBakey Veterans Affairs Medical Center, Houston, TX; 2North Carolina State University, Raleigh, NC; 3Baylor College of Medicine, Houston, TX
Introduction: Management of IBD has transitioned to a treat-to-target paradigm, aiming for defined objective treatment outcomes. C-reactive protein (CRP) has low sensitivity, while stool collection for fecal calprotectin faces challenges with patient adherence. There is a need for more accurate, accessible, and cost-effective blood-based biomarkers in IBD to optimize treat-to-target care.
Methods: We conducted a prospective pilot observational study of IBD patients, including both Crohn’s disease (CD) and Ulcerative Colitis (UC) patients, undergoing endoscopic evaluation for disease activity assessment. Serum protein capillary electrophoresis (SPEP) and C-reactive protein (CRP) were measured pre-procedure before colonoscopy. Wilcoxon rank-sum testing was used to compare SPEP components in g/dL (albumin, alpha-1, alpha-2, beta-1, beta-2, gamma) between patients with endoscopically active disease (eMayo> 1, SES-CD> 2) and those in remission. Logistic regression models were performed to determine discriminatory ability of SPEP components compared to CRP alone.
Results: Our pilot study included 28 patients with complete SPEP, CRP, and endoscopic data: 15 patients with UC and 13 patients with CD. The patient population was predominantly female (71%), White (68%), and non-Hispanic (82%), with an average age of 44 years (SD 16). Among all IBD patients, 46% had endoscopically active disease. In all IBD patients, significant elevations were observed in alpha-1 (95% CI: 0.01-0.12, p=0.009), alpha-2 (95% CI: 0.02-0.24, p=0.03), beta-2 (95% CI: 0.04-0.18, p=0.02), and CRP (95% CI: 0.10-1.0, p=0.01) levels among patients with active endoscopic inflammation (Fig 1A). In all IBD patients, a logistic regression model of CRP had an AUC of 0.79 compared to 0.89 for SPEP components (albumin, alpha-1, alpha-2, beta-1, beta-2, gamma) (Fig 1B). In CD patients, the AUC for CRP was 0.93 and 1.0 for SPEP components; while in UC patients, the AUC for CRP was 0.64 and 0.91 for SPEP components (Fig 1C).
Discussion: Several SPEP components are significantly upregulated in association with endoscopic inflammation in IBD, demonstrating superior discriminatory ability compared to CRP alone. Despite potential overfitting in this limited dataset without an independent testing cohort, SPEP components show clear promise in differentiating endoscopically active IBD. Our goal is to develop a model that integrates both CRP and SPEP components to create an accessible and accurate treat-to-target biomarker for inflammation in IBD.
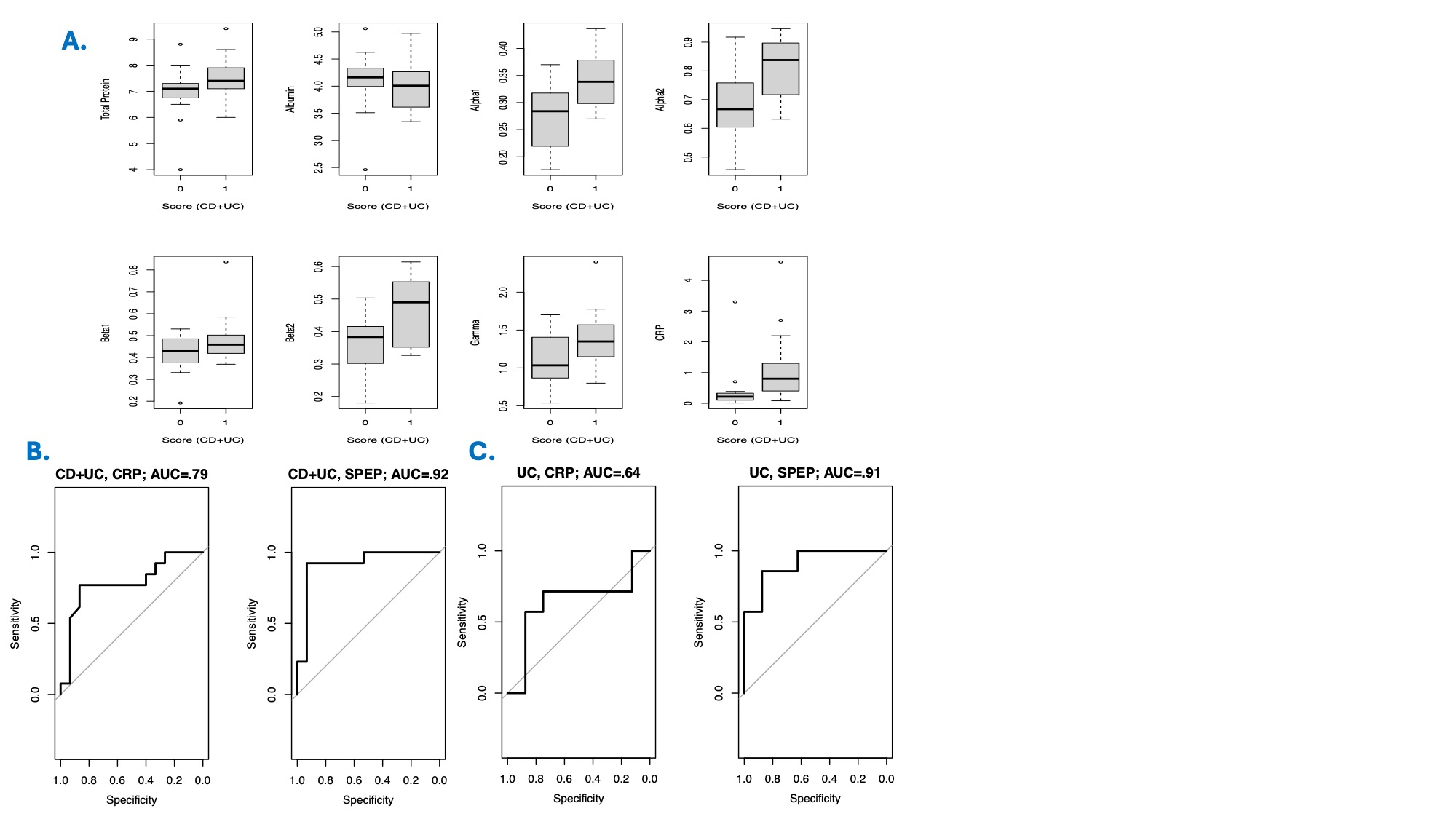
Figure: Figure 1:
A) Box and whisker plots showing the levels of SPEP components and CRP in IBD patients with endoscopic activity (1) versus those in remission (0). B) Logistic regression model of CRP alone versus the SPEP component model for all IBD patients. C) Logistic regression model of CRP alone versus the SPEP component model for UC patients.
A) Box and whisker plots showing the levels of SPEP components and CRP in IBD patients with endoscopic activity (1) versus those in remission (0). B) Logistic regression model of CRP alone versus the SPEP component model for all IBD patients. C) Logistic regression model of CRP alone versus the SPEP component model for UC patients.
Disclosures:
Jared Sninsky indicated no relevant financial relationships.
Ana-Maria Staicu indicated no relevant financial relationships.
Rongrong Huang: Abbott Laboratories – Grant/Research Support. Roche Diagnostic Corporation – Advisory Committee/Board Member.
Adith Ram indicated no relevant financial relationships.
Jason Hou: Abbvie – Grant/Research Support. American Regent – Grant/Research Support. Bristol Myers Squibb – Grant/Research Support. Eli-Lilly – Advisor or Review Panel Member, Grant/Research Support. Janssen – Grant/Research Support. Pfizer – Grant/Research Support. Vedanta – Grant/Research Support.
Jared Sninsky, MD, MSCR1, Ana-Maria Staicu, PhD2, Rongrong Huang, PhD3, Adith Ram, BA3, Jason K. Hou, MD, MS, FACG1. P0958 - Serum Protein Capillary Electrophoresis as a Biomarker for Endoscopic Disease Activity in Inflammatory Bowel Disease: A Prospective Pilot Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

