Sunday Poster Session
Category: IBD
P0878 - Vitamin D Deficiency Is Associated With Worsening Hospitalization Outcomes for Patients With Inflammatory Bowel Disease in the United States
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Saba Altarawneh, MD
The Wright Center for Graduate Medical Education
Huntington, WV
Presenting Author(s)
Saba Altarawneh, MD1, Mohammed El-Dallal, MD, MMSc2, Ean Bills, MD3, Shristee Karki, MD3, Amro Altarawneh, MD3, Ali Algayed, MD2, Yasmeen Obeidat, MD3, Tala Altarawneh, MD3
1The Wright Center for Graduate Medical Education, Huntington, WV; 2Joan C. Edwards School of Medicine, Marshall University, Huntington, WV; 3Marshall University Joan C. Edwards School of Medicine, Huntington, WV
Introduction: Vitamin D deficiency has been linked to Inflammatory bowel diseases (IBD), whether vitamin D deficiency is a cause or a consequence of the disease is not well-known yet. Moreover, there is a critical gap in understanding the potential impact of vitamin D status on disease severity and patient outcomes. This study is exploring the interplay between vitamin D deficiency and hospitalization outcomes in individuals with IBD.
Methods: Utilizing data from the National Inpatient Sample spanning 2016 to 2018, we identified patients with a primary discharge diagnosis of IBD. Within our IBD patient cohort, we distinguished those with a diagnosis of vitamin D deficiency from those without, conducting a thorough comparison based on demographics, Charlson’s comorbidity score, long-term use of antibiotics and steroids, and various hospital characteristics. In our outcome analysis, we mitigated group differences using the Average Treatment Effect methodology with respect to the aforementioned variables.
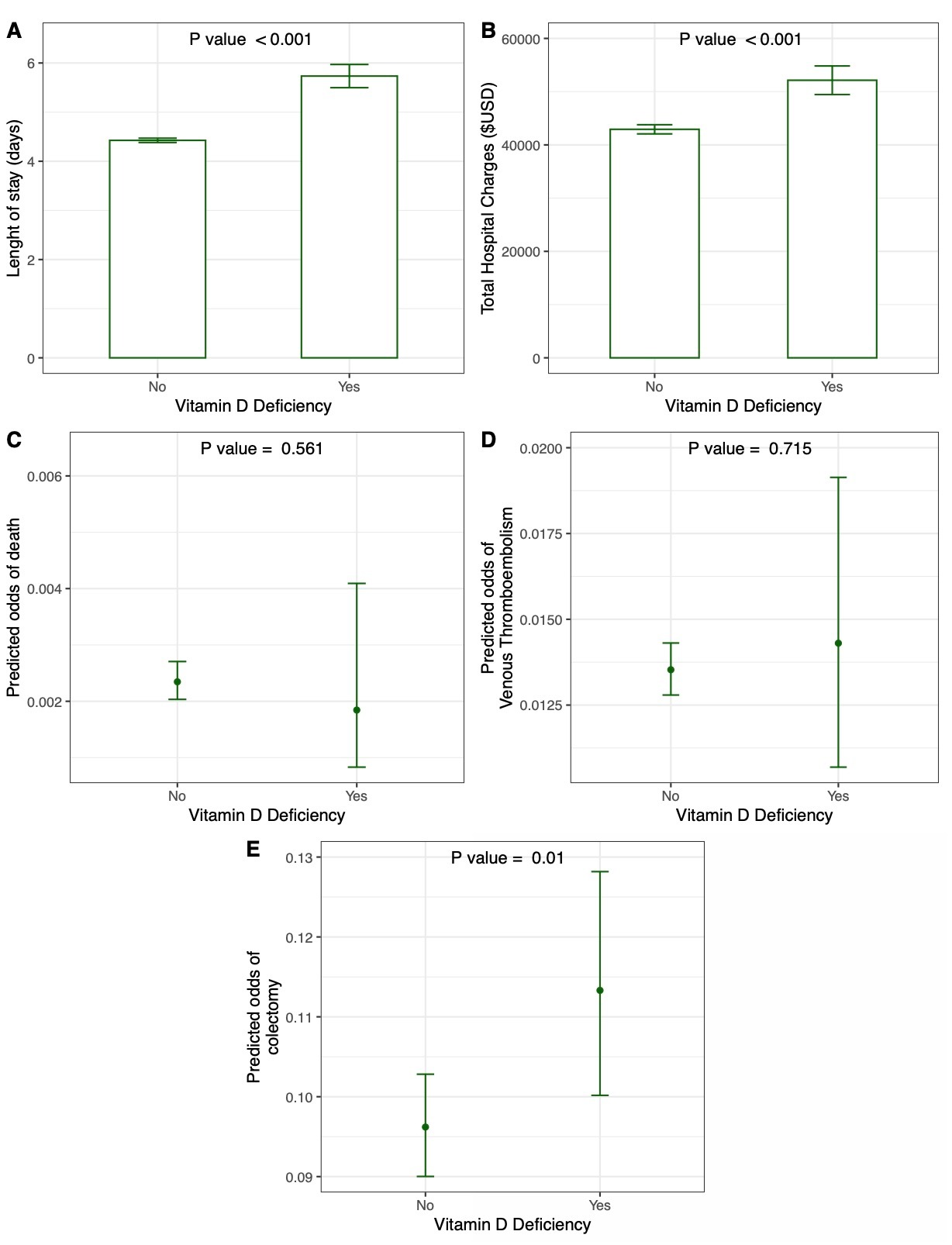
Results: Among 540,650 patients admitted primarily for IBD, 16,310 had a concomitant diagnosis of vitamin D deficiency. Those with both IBD and vitamin D deficiency exhibited a higher likelihood of being female and white and had an increased probability of long-term steroid use. Table 1 summarizes the remaining baseline characteristics. Following adjustments for intergroup differences, our analysis revealed that patients with IBD and vitamin D deficiency experienced a prolonged hospital stay, with a mean difference (MD) of 1.31 days (95% CI 1.07 - 1.55, P < 0.001), elevated hospital charges (MD $9,215.33, 95% CI 6,736.69 - 11,693.96, P < 0.001), and an increased odds ratio (OR) of colectomy (1.18, 95% CI 1.04 - 1.33, P = 0.01). Notably, there were no discernible differences in-hospital mortality (OR 0.79, 95% CI 0.35 - 1.77, P = 0.56) and venous thromboembolism (OR 1.06, 95% CI 0.78 - 1.42, P = 0.76) between the two groups (Figure 1).
Discussion: Vitamin D deficiency is prevalent in IBD patients in multiple studies. Small studies in < 20 patients have shown that vitamin D supplementation has been associated with better outcomes in IBD patients with vitamin deficiency. We studied 16,310 IBD patients with vitamin D deficiency, and we found that vitamin D deficiency in IBD patients has been associated with longer hospital stays, increased hospital charges, and increased odds ratio of colectomy, which emphasizes the need to establish a standard clinical practice to measure vitamin D in this population.
Disclosures:
Saba Altarawneh, MD1, Mohammed El-Dallal, MD, MMSc2, Ean Bills, MD3, Shristee Karki, MD3, Amro Altarawneh, MD3, Ali Algayed, MD2, Yasmeen Obeidat, MD3, Tala Altarawneh, MD3. P0878 - Vitamin D Deficiency Is Associated With Worsening Hospitalization Outcomes for Patients With Inflammatory Bowel Disease in the United States, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1The Wright Center for Graduate Medical Education, Huntington, WV; 2Joan C. Edwards School of Medicine, Marshall University, Huntington, WV; 3Marshall University Joan C. Edwards School of Medicine, Huntington, WV
Introduction: Vitamin D deficiency has been linked to Inflammatory bowel diseases (IBD), whether vitamin D deficiency is a cause or a consequence of the disease is not well-known yet. Moreover, there is a critical gap in understanding the potential impact of vitamin D status on disease severity and patient outcomes. This study is exploring the interplay between vitamin D deficiency and hospitalization outcomes in individuals with IBD.
Methods: Utilizing data from the National Inpatient Sample spanning 2016 to 2018, we identified patients with a primary discharge diagnosis of IBD. Within our IBD patient cohort, we distinguished those with a diagnosis of vitamin D deficiency from those without, conducting a thorough comparison based on demographics, Charlson’s comorbidity score, long-term use of antibiotics and steroids, and various hospital characteristics. In our outcome analysis, we mitigated group differences using the Average Treatment Effect methodology with respect to the aforementioned variables.
Results: Among 540,650 patients admitted primarily for IBD, 16,310 had a concomitant diagnosis of vitamin D deficiency. Those with both IBD and vitamin D deficiency exhibited a higher likelihood of being female and white and had an increased probability of long-term steroid use. Table 1 summarizes the remaining baseline characteristics. Following adjustments for intergroup differences, our analysis revealed that patients with IBD and vitamin D deficiency experienced a prolonged hospital stay, with a mean difference (MD) of 1.31 days (95% CI 1.07 - 1.55, P < 0.001), elevated hospital charges (MD $9,215.33, 95% CI 6,736.69 - 11,693.96, P < 0.001), and an increased odds ratio (OR) of colectomy (1.18, 95% CI 1.04 - 1.33, P = 0.01). Notably, there were no discernible differences in-hospital mortality (OR 0.79, 95% CI 0.35 - 1.77, P = 0.56) and venous thromboembolism (OR 1.06, 95% CI 0.78 - 1.42, P = 0.76) between the two groups (Figure 1).
Discussion: Vitamin D deficiency is prevalent in IBD patients in multiple studies. Small studies in < 20 patients have shown that vitamin D supplementation has been associated with better outcomes in IBD patients with vitamin deficiency. We studied 16,310 IBD patients with vitamin D deficiency, and we found that vitamin D deficiency in IBD patients has been associated with longer hospital stays, increased hospital charges, and increased odds ratio of colectomy, which emphasizes the need to establish a standard clinical practice to measure vitamin D in this population.
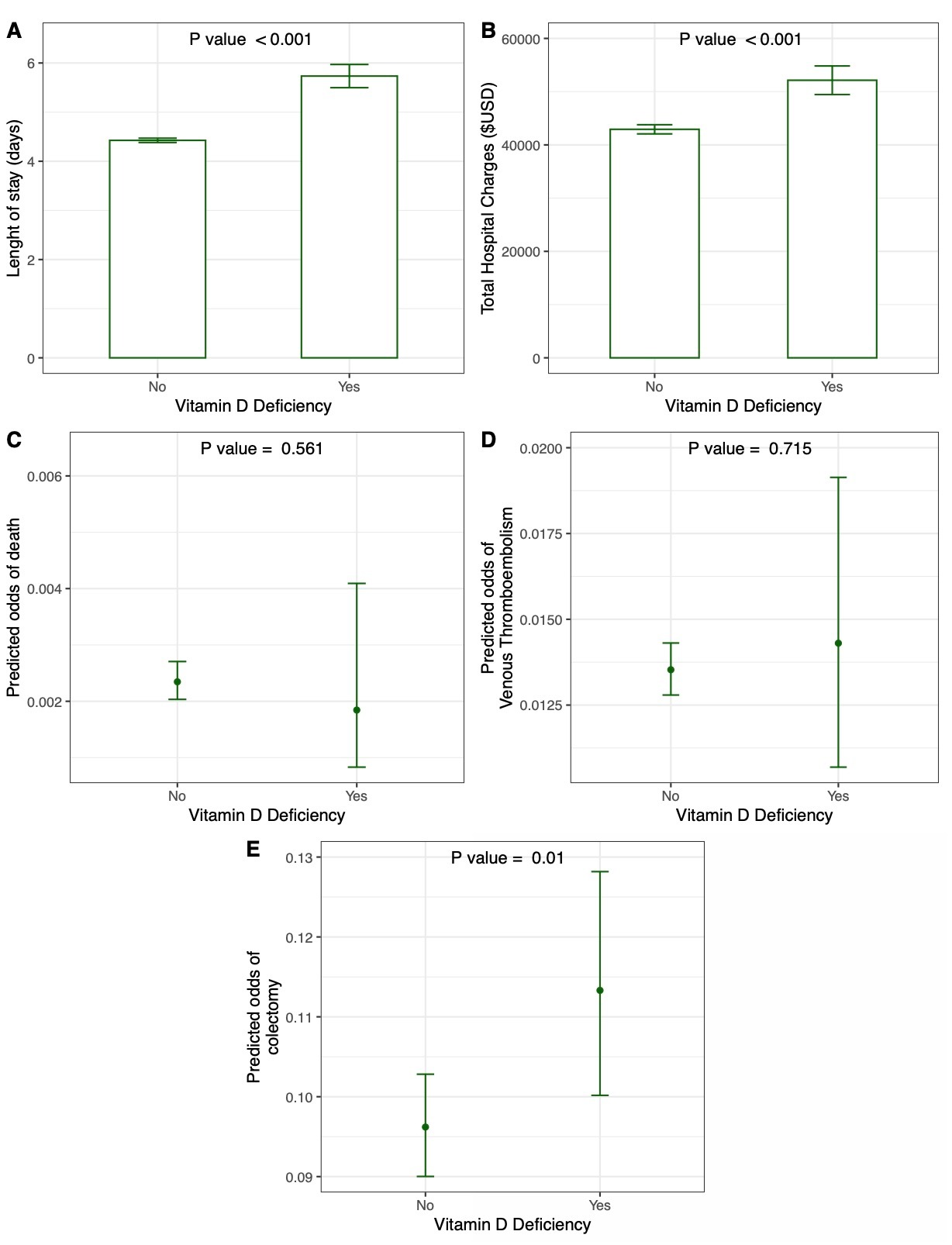
Figure: Figure 1. Hospitalization outcomes for patients with concomitant diagnoses of IBD and vitamin D deficiency compared to patients admitted with IBD without vitamin D deficiency.
Disclosures:
Saba Altarawneh indicated no relevant financial relationships.
Mohammed El-Dallal indicated no relevant financial relationships.
Ean Bills indicated no relevant financial relationships.
Shristee Karki indicated no relevant financial relationships.
Amro Altarawneh indicated no relevant financial relationships.
Ali Algayed indicated no relevant financial relationships.
Yasmeen Obeidat indicated no relevant financial relationships.
Tala Altarawneh indicated no relevant financial relationships.
Saba Altarawneh, MD1, Mohammed El-Dallal, MD, MMSc2, Ean Bills, MD3, Shristee Karki, MD3, Amro Altarawneh, MD3, Ali Algayed, MD2, Yasmeen Obeidat, MD3, Tala Altarawneh, MD3. P0878 - Vitamin D Deficiency Is Associated With Worsening Hospitalization Outcomes for Patients With Inflammatory Bowel Disease in the United States, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
