Sunday Poster Session
Category: IBD
P0883 - Comparative Safety Profiles of Second Line Biologic Therapies in Patients With Moderate to Severe Ulcerative Colitis: A Nationwide Population-Based Cohort Study in the USA
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E

Shu-Yen Emily Chan, MD, MSc
Weiss Memorial Hospital
Chicago, IL
Presenting Author(s)
Emily Shu-Yen Chan, MD, MSc, Johanna Elena Blagoie, MD, Shehzad Ali, MD, Olumuyiwa Idowu, MD
Weiss Memorial Hospital, Chicago, IL
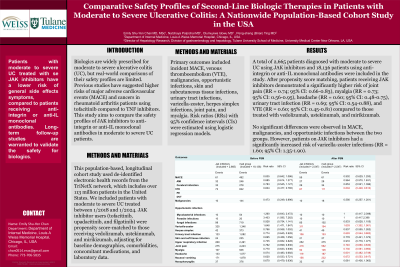
Introduction: Biologics are widely prescribed for moderate to severe ulcerative colitis (UC), but real-world comparisons of their safety profiles are limited. Previous studies suggested higher risks of major adverse cardiovascular events (MACE) and cancers in rheumatoid arthritis patients using tofacitinib compared to TNF inhibitors. This study aims to compare the safety profiles of JAK inhibitors to anti-integrin or anti-IL monoclonal antibodies in moderate to severe UC patients.
Methods: This population-based, longitudinal cohort study used de-identified electronic health records from the TriNetX network, which includes over 113 million patients in the United States. We included patients with moderate to severe UC treated between 1/2018 and 1/2024. JAK inhibitor users (tofacitinib, upadacitinib, and filgotinib) were propensity score-matched to those receiving vedolizumab, ustekinumab, and mirikizumab, adjusting for baseline demographics, comorbidities, concomitant medications, and laboratory data. Primary outcomes included incident MACE, venous thromboembolism (VTE), malignancies, opportunistic infections, skin and subcutaneous tissue infections, urinary tract infections, varicella-zoster, herpes simplex infections, joint pain, and myalgia. Risk ratios (RRs) with 95% confidence intervals (CIs) were estimated using logistic regression models.
Results: A total of 2,665 patients diagnosed with moderate to severe UC using JAK inhibitors and 18,136 patients using anti-integrin or anti-IL monoclonal antibodies were included in the study. After propensity score matching, patients receiving JAK inhibitors demonstrated a significantly higher risk of joint pain (RR = 0.74; 95% CI: 0.66-0.83), myalgia (RR = 0.73; 95% CI: 0.56-0.95), headache (RR = 0.60; 95% CI: 0.48-0.75), urinary tract infection (RR = 0.69; 95% CI: 0.54-0.88), and VTE (RR = 0.60; 95% CI: 0.45-0.81) compared to those treated with vedolizumab, ustekinumab, and mirikizumab. No significant differences were observed in MACE, malignancies, and opportunistic infections between the two groups. However, patients on JAK inhibitors had a significantly increased risk of varicella-zoster infections (RR = 1.60; 95% CI: 1.35-1.90).
Discussion: Patients with moderate to severe UC treated with JAK inhibitors have a lower risk of general side effects symptoms, compared to patients receiving anti-integrin or anti-IL monoclonal antibodies. Long-term follow-up studies are warranted to validate the safety for biologics.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Emily Shu-Yen Chan, MD, MSc, Johanna Elena Blagoie, MD, Shehzad Ali, MD, Olumuyiwa Idowu, MD. P0883 - Comparative Safety Profiles of Second Line Biologic Therapies in Patients With Moderate to Severe Ulcerative Colitis: A Nationwide Population-Based Cohort Study in the USA, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Weiss Memorial Hospital, Chicago, IL
Introduction: Biologics are widely prescribed for moderate to severe ulcerative colitis (UC), but real-world comparisons of their safety profiles are limited. Previous studies suggested higher risks of major adverse cardiovascular events (MACE) and cancers in rheumatoid arthritis patients using tofacitinib compared to TNF inhibitors. This study aims to compare the safety profiles of JAK inhibitors to anti-integrin or anti-IL monoclonal antibodies in moderate to severe UC patients.
Methods: This population-based, longitudinal cohort study used de-identified electronic health records from the TriNetX network, which includes over 113 million patients in the United States. We included patients with moderate to severe UC treated between 1/2018 and 1/2024. JAK inhibitor users (tofacitinib, upadacitinib, and filgotinib) were propensity score-matched to those receiving vedolizumab, ustekinumab, and mirikizumab, adjusting for baseline demographics, comorbidities, concomitant medications, and laboratory data. Primary outcomes included incident MACE, venous thromboembolism (VTE), malignancies, opportunistic infections, skin and subcutaneous tissue infections, urinary tract infections, varicella-zoster, herpes simplex infections, joint pain, and myalgia. Risk ratios (RRs) with 95% confidence intervals (CIs) were estimated using logistic regression models.
Results: A total of 2,665 patients diagnosed with moderate to severe UC using JAK inhibitors and 18,136 patients using anti-integrin or anti-IL monoclonal antibodies were included in the study. After propensity score matching, patients receiving JAK inhibitors demonstrated a significantly higher risk of joint pain (RR = 0.74; 95% CI: 0.66-0.83), myalgia (RR = 0.73; 95% CI: 0.56-0.95), headache (RR = 0.60; 95% CI: 0.48-0.75), urinary tract infection (RR = 0.69; 95% CI: 0.54-0.88), and VTE (RR = 0.60; 95% CI: 0.45-0.81) compared to those treated with vedolizumab, ustekinumab, and mirikizumab. No significant differences were observed in MACE, malignancies, and opportunistic infections between the two groups. However, patients on JAK inhibitors had a significantly increased risk of varicella-zoster infections (RR = 1.60; 95% CI: 1.35-1.90).
Discussion: Patients with moderate to severe UC treated with JAK inhibitors have a lower risk of general side effects symptoms, compared to patients receiving anti-integrin or anti-IL monoclonal antibodies. Long-term follow-up studies are warranted to validate the safety for biologics.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Emily Shu-Yen Chan indicated no relevant financial relationships.
Johanna Elena Blagoie indicated no relevant financial relationships.
Shehzad Ali indicated no relevant financial relationships.
Olumuyiwa Idowu indicated no relevant financial relationships.
Emily Shu-Yen Chan, MD, MSc, Johanna Elena Blagoie, MD, Shehzad Ali, MD, Olumuyiwa Idowu, MD. P0883 - Comparative Safety Profiles of Second Line Biologic Therapies in Patients With Moderate to Severe Ulcerative Colitis: A Nationwide Population-Based Cohort Study in the USA, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
