Sunday Poster Session
Category: IBD
P0889 - A Nationwide Analysis of Prevalence, Trends, and Cardiovascular Outcomes Associated With Metabolically Healthy and Unhealthy Obesity in Elderly IBD Patients (2016- 2020)
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Rishika Trivedi, MD
DHR Health
Edinburg, TX
Presenting Author(s)
Rishika Trivedi, MD1, Boney Lapsiwala, MD2, Sahiljot Bhupal, MBBS3, Pranav Chalasani, MD4, Amrutha Yalla, MBBS5, Sahana Bopparaju, 6, Shreyans Doshi, MD7, Rupak Desai, MBBS8
1DHR Health, Edinburg, TX; 2Medical City Arlington, Denton, TX; 3Dayanand Medical College and Hospital, Chicago, IL; 4Wayne State University School of Medicine / Ascension Providence Rochester Hospital, Rochester, MI; 5Jawaharlal Nehru Medical College, Belagavi, Karnataka, India; 6Osmania General Hospital and Medical College, Hyderabad, Telangana, India; 7Wake Forest University School of Medicine, Charlotte, NC; 8Outcomes Research, Atlanta, GA
Introduction:
Inflammatory bowel disease (IBD) is a growing global healthcare problem. Despite obesity's link to inflammation, a recent meta-analysis found an inverse association between obesity & IBD incidence. Global rise in obesity highlights the importance of understanding its phenotypes, particularly metabolically healthy obesity (MHO) and metabolically unhealthy obesity (MUHO). We aim to analyze prevalence, trends & impact of MHO and MUHO on cardiovascular events in elderly patients hospitalized with IBD.
Methods:
National Inpatient sample 2016-2020 was queried using ICD-10 codes to identify inpatient encounters of obese geriatric patients (age >65). A 1:1:1 propensity score-matched analysis was performed to obtain balanced MHO, MUHO and non-obese cohorts. Multivariate logistic regression was used to analyze all-cause mortality (ACM), major adverse cardiovascular events (MACE), acute myocardial infarction, cardiac arrest, acute ischemic stroke (AIS) and venous thromboembolism (VTE).
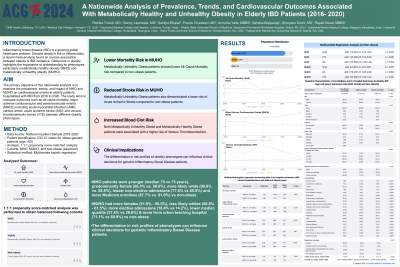
Results:
Out of 541,800 elderly IBD admission, (87.6%) were non-obese, (1%) MHO & (11.4%) MUHO. MHO had higher prevalence of ACM (3.6%) & VTE (3.7%) as compared to non-obese with higher MACE (6.4%, p< 0.001). MHO patients were younger (median 70 vs 75 years), predominantly female (66.3% vs. 56.6%), more likely white (90.8% vs. 88.9%), lesser non-elective admissions (77.6% vs 85.8%) and Medicare enrollees (87.7% vs. 91.0%) vs non-obese. Over 5 years, MUHO had increasing crude rates with difference of 0.8% in ACM, 2.1% in MACE and 0.8% in VTE, with more females (61.9% - 56.5%), less likely whites (56.8% - 61.5%), more elective admissions (18.4% vs 14.2%), lower median quartile (27.4% vs 26.6%) & from urban teaching hospital (71.1% vs 69.9%) vs non-obese. Multivariable regression analysis showed MHO had higher odds for ACM (aOR 1.10, 95%CI: 0.79-1.54, p 0.007), VTE (aOR 1.45, 95%Cl 1.03-2.04, p 0.001) and lower AIS (aOR 0.79, 95%Cl 0.39-1.59, p-0.005), while MUHO had lower odds for ACM (aOR 0.8, 95%Cl 0.70-0.92, p 0.007), AIS (aOR 0.76, 95%Cl 0.65-0.90, p 0.005) and higher VTE (aOR 1.25, 95%Cl 1.09-1.44) as compared to non-obese. The median cost of admission was higher in MHO ($48,760) and MUHO ($47,943) vs non-obese ($47,690, p< 0.001).
Discussion:
The analysis showed, MUHO was associated with lower ACM & AIS risk than non-obese. In contrast, both MUHO and MHO were associated with a higher risk of VTE. The differentiation in risk profiles of phenotypes can influence clinical decisions for geriatric IBD patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Rishika Trivedi, MD1, Boney Lapsiwala, MD2, Sahiljot Bhupal, MBBS3, Pranav Chalasani, MD4, Amrutha Yalla, MBBS5, Sahana Bopparaju, 6, Shreyans Doshi, MD7, Rupak Desai, MBBS8. P0889 - A Nationwide Analysis of Prevalence, Trends, and Cardiovascular Outcomes Associated With Metabolically Healthy and Unhealthy Obesity in Elderly IBD Patients (2016- 2020), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1DHR Health, Edinburg, TX; 2Medical City Arlington, Denton, TX; 3Dayanand Medical College and Hospital, Chicago, IL; 4Wayne State University School of Medicine / Ascension Providence Rochester Hospital, Rochester, MI; 5Jawaharlal Nehru Medical College, Belagavi, Karnataka, India; 6Osmania General Hospital and Medical College, Hyderabad, Telangana, India; 7Wake Forest University School of Medicine, Charlotte, NC; 8Outcomes Research, Atlanta, GA
Introduction:
Inflammatory bowel disease (IBD) is a growing global healthcare problem. Despite obesity's link to inflammation, a recent meta-analysis found an inverse association between obesity & IBD incidence. Global rise in obesity highlights the importance of understanding its phenotypes, particularly metabolically healthy obesity (MHO) and metabolically unhealthy obesity (MUHO). We aim to analyze prevalence, trends & impact of MHO and MUHO on cardiovascular events in elderly patients hospitalized with IBD.
Methods:
National Inpatient sample 2016-2020 was queried using ICD-10 codes to identify inpatient encounters of obese geriatric patients (age >65). A 1:1:1 propensity score-matched analysis was performed to obtain balanced MHO, MUHO and non-obese cohorts. Multivariate logistic regression was used to analyze all-cause mortality (ACM), major adverse cardiovascular events (MACE), acute myocardial infarction, cardiac arrest, acute ischemic stroke (AIS) and venous thromboembolism (VTE).
Results:
Out of 541,800 elderly IBD admission, (87.6%) were non-obese, (1%) MHO & (11.4%) MUHO. MHO had higher prevalence of ACM (3.6%) & VTE (3.7%) as compared to non-obese with higher MACE (6.4%, p< 0.001). MHO patients were younger (median 70 vs 75 years), predominantly female (66.3% vs. 56.6%), more likely white (90.8% vs. 88.9%), lesser non-elective admissions (77.6% vs 85.8%) and Medicare enrollees (87.7% vs. 91.0%) vs non-obese. Over 5 years, MUHO had increasing crude rates with difference of 0.8% in ACM, 2.1% in MACE and 0.8% in VTE, with more females (61.9% - 56.5%), less likely whites (56.8% - 61.5%), more elective admissions (18.4% vs 14.2%), lower median quartile (27.4% vs 26.6%) & from urban teaching hospital (71.1% vs 69.9%) vs non-obese. Multivariable regression analysis showed MHO had higher odds for ACM (aOR 1.10, 95%CI: 0.79-1.54, p 0.007), VTE (aOR 1.45, 95%Cl 1.03-2.04, p 0.001) and lower AIS (aOR 0.79, 95%Cl 0.39-1.59, p-0.005), while MUHO had lower odds for ACM (aOR 0.8, 95%Cl 0.70-0.92, p 0.007), AIS (aOR 0.76, 95%Cl 0.65-0.90, p 0.005) and higher VTE (aOR 1.25, 95%Cl 1.09-1.44) as compared to non-obese. The median cost of admission was higher in MHO ($48,760) and MUHO ($47,943) vs non-obese ($47,690, p< 0.001).
Discussion:
The analysis showed, MUHO was associated with lower ACM & AIS risk than non-obese. In contrast, both MUHO and MHO were associated with a higher risk of VTE. The differentiation in risk profiles of phenotypes can influence clinical decisions for geriatric IBD patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Rishika Trivedi indicated no relevant financial relationships.
Boney Lapsiwala indicated no relevant financial relationships.
Sahiljot Bhupal indicated no relevant financial relationships.
Pranav Chalasani indicated no relevant financial relationships.
Amrutha Yalla indicated no relevant financial relationships.
Sahana Bopparaju indicated no relevant financial relationships.
Shreyans Doshi indicated no relevant financial relationships.
Rupak Desai indicated no relevant financial relationships.
Rishika Trivedi, MD1, Boney Lapsiwala, MD2, Sahiljot Bhupal, MBBS3, Pranav Chalasani, MD4, Amrutha Yalla, MBBS5, Sahana Bopparaju, 6, Shreyans Doshi, MD7, Rupak Desai, MBBS8. P0889 - A Nationwide Analysis of Prevalence, Trends, and Cardiovascular Outcomes Associated With Metabolically Healthy and Unhealthy Obesity in Elderly IBD Patients (2016- 2020), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

