Sunday Poster Session
Category: IBD
P0890 - Outcomes in Inflammatory Bowel Disease After Percutaneous Coronary Intervention: A National Readmission Database Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- UB
Umesh Bhagat, MD
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Prabhat Kumar, MD1, Umesh Bhagat, MD1, Archana Kharel, MD1, Stephen J. Bickston, MD, FACG2
1Cleveland Clinic Foundation, Cleveland, OH; 2Virginia Commonwealth University Health System, Richmond, VA
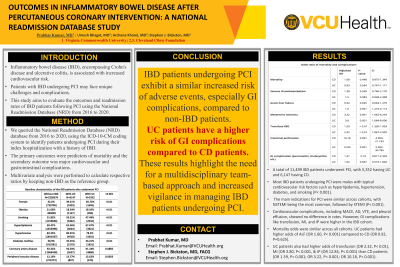
Introduction: Inflammatory bowel disease (IBD), encompassing Crohn's disease and ulcerative colitis, is associated with increased cardiovascular risk. Patients with IBD undergoing percutaneous coronary intervention (PCI) may face unique challenges and complications. This study aims to evaluate the outcomes and readmission rates of IBD patients following PCI using the National Readmission Database (NRD) from 2016 to 2020.
Methods: We queried the National Readmission Database (NRD) database from 2016 to 2020, using the ICD-10-CM coding system to identify patients undergoing PCI during their index hospitalization with a history of IBD. The primary outcomes were predictors of mortality and the secondary outcome was major cardiovascular and gastrointestinal complications. Analysis was performed with STATA software. T-tests were used for continuous variables, and chi-square tests were used for categorical variables. Multivariate analysis were performed to calculate respective ratios by keeping non-IBD as the reference group.
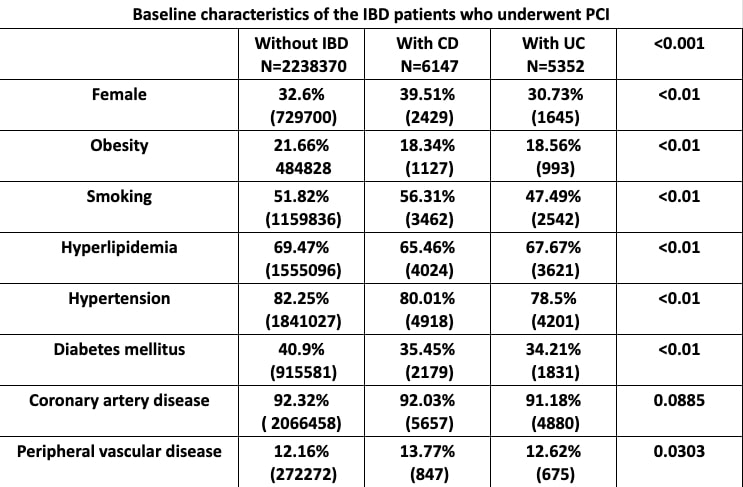
Results: A total of 11,499 IBD patients underwent PCI, with 5,352 having Ulcerative Colitis (UC) and 6,147 having Crohn's Disease (CD). Most IBD patients undergoing PCI were males with typical cardiovascular risk factors such as hyperlipidemia, hypertension, diabetes, and smoking (P< 0.001). The main indications for PCI were similar across cohorts, with NSTEMI being the most common, followed by STEMI (P< 0.001). Cardiovascular complications, including MACE, aortic dissection, VTE, and pleural effusion, showed no difference in rates. However, GI complications like transfusion, mesenteric ischemia, and intestinal perforation were higher in the IBD cohort. Mortality odds were similar across all cohorts. UC patients had higher odds of acute liver failure (OR 1.60, P< 0.001) compared to CD (OR 0.92, P=0.625). UC patients also had higher odds of transfusion (OR 2.32, P< 0.01), mesenteric ischemia (OR 3.80, P< 0.001), and intestinal perforation (OR 12.84, P< 0.001) than CD patients (OR 1.59, P< 0.001; OR 3.22, P< 0.001; OR 10.18, P< 0.001).
Discussion: IBD patients undergoing PCI exhibit a similar increased risk of adverse events, especially GI complications, compared to non-IBD patients. Subgroup analysis shows UC patients have a higher risk of GI complications compared to CD patients. These results highlight the need for a multidisciplinary team-based approach and increased vigilance in managing IBD patients undergoing PCI.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Prabhat Kumar, MD1, Umesh Bhagat, MD1, Archana Kharel, MD1, Stephen J. Bickston, MD, FACG2. P0890 - Outcomes in Inflammatory Bowel Disease After Percutaneous Coronary Intervention: A National Readmission Database Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2Virginia Commonwealth University Health System, Richmond, VA
Introduction: Inflammatory bowel disease (IBD), encompassing Crohn's disease and ulcerative colitis, is associated with increased cardiovascular risk. Patients with IBD undergoing percutaneous coronary intervention (PCI) may face unique challenges and complications. This study aims to evaluate the outcomes and readmission rates of IBD patients following PCI using the National Readmission Database (NRD) from 2016 to 2020.
Methods: We queried the National Readmission Database (NRD) database from 2016 to 2020, using the ICD-10-CM coding system to identify patients undergoing PCI during their index hospitalization with a history of IBD. The primary outcomes were predictors of mortality and the secondary outcome was major cardiovascular and gastrointestinal complications. Analysis was performed with STATA software. T-tests were used for continuous variables, and chi-square tests were used for categorical variables. Multivariate analysis were performed to calculate respective ratios by keeping non-IBD as the reference group.
Results: A total of 11,499 IBD patients underwent PCI, with 5,352 having Ulcerative Colitis (UC) and 6,147 having Crohn's Disease (CD). Most IBD patients undergoing PCI were males with typical cardiovascular risk factors such as hyperlipidemia, hypertension, diabetes, and smoking (P< 0.001). The main indications for PCI were similar across cohorts, with NSTEMI being the most common, followed by STEMI (P< 0.001). Cardiovascular complications, including MACE, aortic dissection, VTE, and pleural effusion, showed no difference in rates. However, GI complications like transfusion, mesenteric ischemia, and intestinal perforation were higher in the IBD cohort. Mortality odds were similar across all cohorts. UC patients had higher odds of acute liver failure (OR 1.60, P< 0.001) compared to CD (OR 0.92, P=0.625). UC patients also had higher odds of transfusion (OR 2.32, P< 0.01), mesenteric ischemia (OR 3.80, P< 0.001), and intestinal perforation (OR 12.84, P< 0.001) than CD patients (OR 1.59, P< 0.001; OR 3.22, P< 0.001; OR 10.18, P< 0.001).
Discussion: IBD patients undergoing PCI exhibit a similar increased risk of adverse events, especially GI complications, compared to non-IBD patients. Subgroup analysis shows UC patients have a higher risk of GI complications compared to CD patients. These results highlight the need for a multidisciplinary team-based approach and increased vigilance in managing IBD patients undergoing PCI.
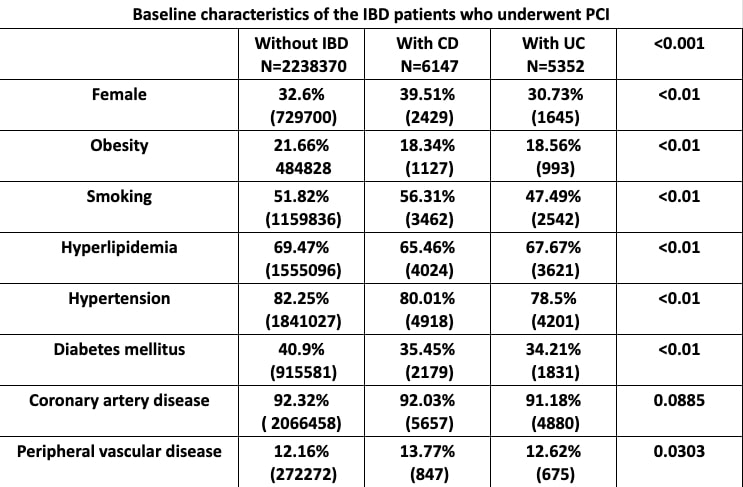
Figure: Image: Baseline characteristics of the IBD patients who underwent PCI.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Prabhat Kumar indicated no relevant financial relationships.
Umesh Bhagat indicated no relevant financial relationships.
Archana Kharel indicated no relevant financial relationships.
Stephen Bickston indicated no relevant financial relationships.
Prabhat Kumar, MD1, Umesh Bhagat, MD1, Archana Kharel, MD1, Stephen J. Bickston, MD, FACG2. P0890 - Outcomes in Inflammatory Bowel Disease After Percutaneous Coronary Intervention: A National Readmission Database Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
