Sunday Poster Session
Category: GI Bleeding
P0784 - Uncovering a Rare Cause of Lower Gastrointestinal Bleeding
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
Khalid Aloum, MD
St. Barnabas Hospital
Bronx, NY
Presenting Author(s)
Khalid Aloum, MD1, Amr Dokmak, MD2, Camelia Ciobanu, MD2, Ali Wakil, MD2, Suresh Nayudu, MD, FACG1
1St. Barnabas Hospital, Bronx, NY; 2Brooklyn Hospital Center, Brooklyn, NY
Introduction: Lower gastrointestinal (GI) bleeding can stem from a wide range of causes, making thorough investigation essential. In this intriguing case, we uncover a rare cause of lower GI bleeding.
Case Description/Methods: A 33-year-old male with no significant past medical history presented to the emergency room with a 3 week history of hematochezia, lower abdominal pain during defecation and unintentional weight loss of 20 lbs. He denied vomiting, fever, sick contact, travel, recent antibiotic use, or history of hemorrhoids.
Physical exam was remarkable for blood on digital rectal examination. Labs were remarkable for a hemoglobin level of 5.5 g/dL and a white blood count of 9.5 x10ˆ9/L. The patient was transfused with packed red blood cells. Stool studies revealed elevated WBC. Stool culture was negative and no ova, cysts, or parasites were reported.
Abdominal CT revealed diffuse thickening of the wall of the descending colon, sigmoid colon, and rectum. Colonoscopy was performed and showed pan-colonic inflammation from the rectum to the cecum which led to a primitive diagnosis of inflammatory bowel disease. Biopsies were obtained and the patient was started on oral and rectal mesalamine. Pathology revealed numerous parasitic ova involving the colon, consistent with schistosomiasis. Praziquantel was prescribed and mesalamine was discontinued. He later reported resolution of prior GI symptoms and weight loss. He did not follow up for a repeat colonoscopy.
Discussion: Schistosomiasis is most prevalent in sub-Saharan Africa, with over 200 million people estimated to be infected globally. Depending on the type of worm, it may migrate to the mesenteric venules of the small and large intestine or the vesical venous plexus.
Eggs released by adult worms can invade local tissues, release toxins and enzymes provoking a TH-2-mediated immune response leading to inflammation and ulceration.
Intestinal schistosomiasis can cause abdominal pain, poor appetite, and diarrhea. However, in heavy infection, chronic colonic ulceration may lead to intestinal bleeding and iron deficiency anemia.
This case highlights the importance of considering a broad spectrum of differential diagnoses of lower GI bleeding, especially in patients with relevant exposure history. Prompt diagnosis and appropriate treatment can lead to significant improvement in symptoms and prevent further complications.

Disclosures:
Khalid Aloum, MD1, Amr Dokmak, MD2, Camelia Ciobanu, MD2, Ali Wakil, MD2, Suresh Nayudu, MD, FACG1. P0784 - Uncovering a Rare Cause of Lower Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1St. Barnabas Hospital, Bronx, NY; 2Brooklyn Hospital Center, Brooklyn, NY
Introduction: Lower gastrointestinal (GI) bleeding can stem from a wide range of causes, making thorough investigation essential. In this intriguing case, we uncover a rare cause of lower GI bleeding.
Case Description/Methods: A 33-year-old male with no significant past medical history presented to the emergency room with a 3 week history of hematochezia, lower abdominal pain during defecation and unintentional weight loss of 20 lbs. He denied vomiting, fever, sick contact, travel, recent antibiotic use, or history of hemorrhoids.
Physical exam was remarkable for blood on digital rectal examination. Labs were remarkable for a hemoglobin level of 5.5 g/dL and a white blood count of 9.5 x10ˆ9/L. The patient was transfused with packed red blood cells. Stool studies revealed elevated WBC. Stool culture was negative and no ova, cysts, or parasites were reported.
Abdominal CT revealed diffuse thickening of the wall of the descending colon, sigmoid colon, and rectum. Colonoscopy was performed and showed pan-colonic inflammation from the rectum to the cecum which led to a primitive diagnosis of inflammatory bowel disease. Biopsies were obtained and the patient was started on oral and rectal mesalamine. Pathology revealed numerous parasitic ova involving the colon, consistent with schistosomiasis. Praziquantel was prescribed and mesalamine was discontinued. He later reported resolution of prior GI symptoms and weight loss. He did not follow up for a repeat colonoscopy.
Discussion: Schistosomiasis is most prevalent in sub-Saharan Africa, with over 200 million people estimated to be infected globally. Depending on the type of worm, it may migrate to the mesenteric venules of the small and large intestine or the vesical venous plexus.
Eggs released by adult worms can invade local tissues, release toxins and enzymes provoking a TH-2-mediated immune response leading to inflammation and ulceration.
Intestinal schistosomiasis can cause abdominal pain, poor appetite, and diarrhea. However, in heavy infection, chronic colonic ulceration may lead to intestinal bleeding and iron deficiency anemia.
This case highlights the importance of considering a broad spectrum of differential diagnoses of lower GI bleeding, especially in patients with relevant exposure history. Prompt diagnosis and appropriate treatment can lead to significant improvement in symptoms and prevent further complications.

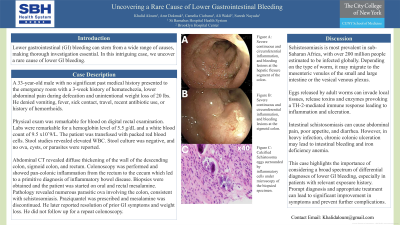
Figure: Figure A: Severe continuous and circumferential inflammation, and bleeding lesions at the hepatic flexure segment of the colon.
Figure B: Severe continuous and circumferential inflammation, and bleeding lesions at the sigmoid colon.
Figure C: Calcified Schistosoma eggs surrounded by inflammatory cells under microscopy of the biopsied specimen.
Figure B: Severe continuous and circumferential inflammation, and bleeding lesions at the sigmoid colon.
Figure C: Calcified Schistosoma eggs surrounded by inflammatory cells under microscopy of the biopsied specimen.
Disclosures:
Khalid Aloum indicated no relevant financial relationships.
Amr Dokmak indicated no relevant financial relationships.
Camelia Ciobanu indicated no relevant financial relationships.
Ali Wakil indicated no relevant financial relationships.
Suresh Nayudu indicated no relevant financial relationships.
Khalid Aloum, MD1, Amr Dokmak, MD2, Camelia Ciobanu, MD2, Ali Wakil, MD2, Suresh Nayudu, MD, FACG1. P0784 - Uncovering a Rare Cause of Lower Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
