Sunday Poster Session
Category: GI Bleeding
P0788 - Isolated Gastric Varices in the Setting of Granulomatosis With Polyangiitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

William Nowlin, DO
University of Oklahoma College of Medicine
Tulsa, OK
Presenting Author(s)
William Nowlin, DO1, Brock Orme, DO1, Collin Beckstrom, DO2, Robert Aran, DO2, Amanda Gibson, MD, MPH1
1University of Oklahoma College of Medicine, Tulsa, OK; 2Oklahoma State University College of Osteopathic Medicine, Tulsa, OK
Introduction: Gastric varices (GV) can result in life threatening blood loss due to a high propensity for severe bleeding. This makes prevention, identification, and treatment of gastric varices critical. GV are classified into gastroesophageal varices or isolated gastric varices (IGV) if limited to the stomach. GV may be caused by a number of conditions that cause portal hypertension. Splenic vein thrombosis (SVT) is a common cause of noncirrhotic portal hypertension. SVT is often seen in chronic inflammatory states due to increased risk of venous thrombosis associated with these conditions. Among these conditions is granulomatosis with polyangiitis (GPA), an antineutrophilic cytoplasmic antibody associated vasculopathy. Patients with GPA have an increased risk for venous thromboembolic events which may increase the risk of SVT and therefore varices. We present a case where IGV were identified in a patient with GPA.
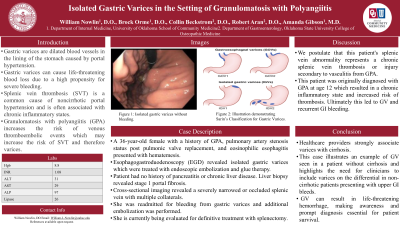
Case Description/Methods: A 36-year-old female with a history of GPA, pulmonary artery stenosis status post pulmonic valve replacement, and eosinophilic esophagitis presented with hematemesis. Urgent esophagogastroduodenoscopy (EGD) was performed, showing IGV which were treated with endoscopic embolization and glue therapy. She had no history of chronic liver disease with normal liver appearance on imaging. Following hospitalization, she had a liver biopsy that demonstrated macrovesicular steatosis and stage 1 portal fibrosis. She had no history of acute pancreatitis or signs of chronic pancreatitis on imaging. Cross sectional imaging revealed a severely narrowed or occluded splenic vein with multiple collaterals. It is postulated that this patient's splenic vein abnormality represents a chronic splenic vein thrombosis or injury secondary to vasculitis from GPA. She was readmitted for bleeding from GV and additional embolizations were performed. She is currently being evaluated for definitive treatment with splenectomy.
Discussion: Healthcare providers strongly associate varices with cirrhosis. This case illustrates an example of GV seen in a patient without cirrhosis and highlights the need for clinicians to include varices on the differential in non-cirrhotic patients presenting with upper GI bleeds. This patient was originally diagnosed with GPA at age 12 which resulted in a chronic inflammatory state and increased risk of thrombosis, ultimately leading to GV and GI bleeding. GV can result in life threatening hemorrhage, making awareness and prompt diagnosis essential for patient survival.
Disclosures:
William Nowlin, DO1, Brock Orme, DO1, Collin Beckstrom, DO2, Robert Aran, DO2, Amanda Gibson, MD, MPH1. P0788 - Isolated Gastric Varices in the Setting of Granulomatosis With Polyangiitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Oklahoma College of Medicine, Tulsa, OK; 2Oklahoma State University College of Osteopathic Medicine, Tulsa, OK
Introduction: Gastric varices (GV) can result in life threatening blood loss due to a high propensity for severe bleeding. This makes prevention, identification, and treatment of gastric varices critical. GV are classified into gastroesophageal varices or isolated gastric varices (IGV) if limited to the stomach. GV may be caused by a number of conditions that cause portal hypertension. Splenic vein thrombosis (SVT) is a common cause of noncirrhotic portal hypertension. SVT is often seen in chronic inflammatory states due to increased risk of venous thrombosis associated with these conditions. Among these conditions is granulomatosis with polyangiitis (GPA), an antineutrophilic cytoplasmic antibody associated vasculopathy. Patients with GPA have an increased risk for venous thromboembolic events which may increase the risk of SVT and therefore varices. We present a case where IGV were identified in a patient with GPA.
Case Description/Methods: A 36-year-old female with a history of GPA, pulmonary artery stenosis status post pulmonic valve replacement, and eosinophilic esophagitis presented with hematemesis. Urgent esophagogastroduodenoscopy (EGD) was performed, showing IGV which were treated with endoscopic embolization and glue therapy. She had no history of chronic liver disease with normal liver appearance on imaging. Following hospitalization, she had a liver biopsy that demonstrated macrovesicular steatosis and stage 1 portal fibrosis. She had no history of acute pancreatitis or signs of chronic pancreatitis on imaging. Cross sectional imaging revealed a severely narrowed or occluded splenic vein with multiple collaterals. It is postulated that this patient's splenic vein abnormality represents a chronic splenic vein thrombosis or injury secondary to vasculitis from GPA. She was readmitted for bleeding from GV and additional embolizations were performed. She is currently being evaluated for definitive treatment with splenectomy.
Discussion: Healthcare providers strongly associate varices with cirrhosis. This case illustrates an example of GV seen in a patient without cirrhosis and highlights the need for clinicians to include varices on the differential in non-cirrhotic patients presenting with upper GI bleeds. This patient was originally diagnosed with GPA at age 12 which resulted in a chronic inflammatory state and increased risk of thrombosis, ultimately leading to GV and GI bleeding. GV can result in life threatening hemorrhage, making awareness and prompt diagnosis essential for patient survival.
Disclosures:
William Nowlin indicated no relevant financial relationships.
Brock Orme indicated no relevant financial relationships.
Collin Beckstrom indicated no relevant financial relationships.
Robert Aran indicated no relevant financial relationships.
Amanda Gibson indicated no relevant financial relationships.
William Nowlin, DO1, Brock Orme, DO1, Collin Beckstrom, DO2, Robert Aran, DO2, Amanda Gibson, MD, MPH1. P0788 - Isolated Gastric Varices in the Setting of Granulomatosis With Polyangiitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
