Sunday Poster Session
Category: GI Bleeding
P0796 - Blakemore Tamponade for Life Threatening Rectal Varices Bleeding
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- AB
Angela Barnes, MD, MBChB
Medical College of Georgia at Augusta University
Augusta, GA
Presenting Author(s)
Angela Barnes, MD, MBChB1, Navkiran Randhawa, DO1, Gautam Maddineni, MD2, Harkanwar Gill, MBBS1, Satish S. C.. Rao, MD, PhD3
1Medical College of Georgia at Augusta University, Augusta, GA; 2Florida State University, Cape Coral, FL; 3Medical College of Georgia, Augusta University, Augusta, GA
Introduction: Esophageal variceal bleeding is a life-threatening manifestation of cirrhosis. However, rectal variceal bleeding is rare and there are no established guidelines for its management. We present a case of severe hematochezia secondary to rectal varices, managed with a Sengstaken-Blakemore tube.
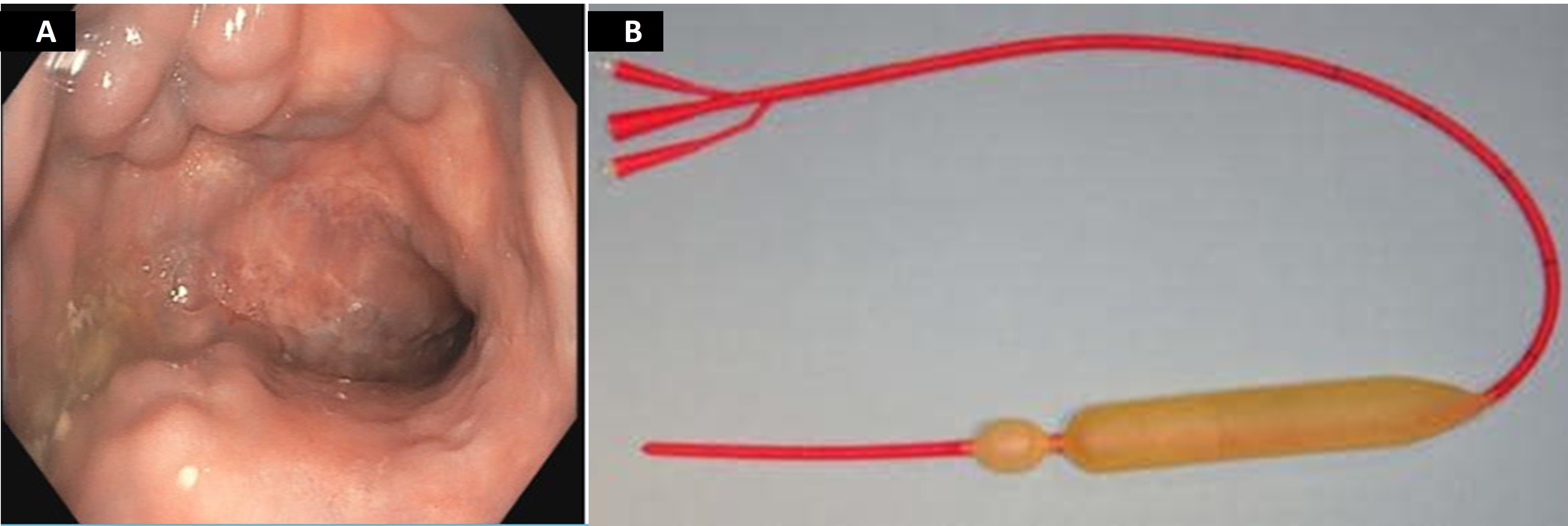
Case Description/Methods: A 67-year-old male with a history of decompensated cirrhosis, refractory ascites and transjugular intrahepatic portosystemic shunt (TIPS), presented with hematochezia. He was hemodynamically stable with a hemoglobin of 11.6g/dl, platelets of 197000/mm3, INR 1.4, MELD 3.0 score of 18 and a Child Pugh B. A doppler abdominal ultrasound revealed nonocclusive thrombus of TIPS. A follow up CT angiogram showed partially occluded TIPS, portal vein, and majority of the SMV. An upper endoscopy revealed no varices. Colonoscopy revealed large rectal varices that were felt to be too large for banding. The patient was recommended for TIPS balloon angioplasty and underwent thrombectomy with post intervention portal venous gradient of 14 mm (from 30 mmHg). However, during the procedure of balloon-occluded retrograde transvenous obliteration (BRTO), the patient developed atrial flutter and the procedure was aborted. Post procedure he developed massive hematochezia requiring transfusion. A bedside flexible sigmoidoscopy revealed large amount of rectal blood with clots, most likely bleeding from the rectal varices and precluding adequate visualization. A Sengstaken-Blakemore tube was inserted and inflated with 200mls of saline, into the rectum with complete resolution of bleeding. The balloon was left in place for about 6 hours and then removed with no further bleeding. The patient was able to undergo BRTO the following day.
Discussion: Various therapeutic interventions including endoscopic variceal ligation and percutaneous transvenous obliteration have been proposed to control significant rectal variceal bleeding. However, they may not be technically feasible with severe variceal bleeding. Under these circumstances, the use of balloon tamponade merits consideration. Although this is effective in controlling 90% of esophageal variceal hemorrhage, its use for rectal varices is not widely reported. Sengstaken-Blakemore tube can be used as a temporizing rescue therapy for rectal varices not amendable to endoscopic therapy. We advocate for the use of this device as a bridging measure for rectal hemorrhage while awaiting definite therapy, and that GI fellows should receive training in its use.
Disclosures:
Angela Barnes, MD, MBChB1, Navkiran Randhawa, DO1, Gautam Maddineni, MD2, Harkanwar Gill, MBBS1, Satish S. C.. Rao, MD, PhD3. P0796 - Blakemore Tamponade for Life Threatening Rectal Varices Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Medical College of Georgia at Augusta University, Augusta, GA; 2Florida State University, Cape Coral, FL; 3Medical College of Georgia, Augusta University, Augusta, GA
Introduction: Esophageal variceal bleeding is a life-threatening manifestation of cirrhosis. However, rectal variceal bleeding is rare and there are no established guidelines for its management. We present a case of severe hematochezia secondary to rectal varices, managed with a Sengstaken-Blakemore tube.
Case Description/Methods: A 67-year-old male with a history of decompensated cirrhosis, refractory ascites and transjugular intrahepatic portosystemic shunt (TIPS), presented with hematochezia. He was hemodynamically stable with a hemoglobin of 11.6g/dl, platelets of 197000/mm3, INR 1.4, MELD 3.0 score of 18 and a Child Pugh B. A doppler abdominal ultrasound revealed nonocclusive thrombus of TIPS. A follow up CT angiogram showed partially occluded TIPS, portal vein, and majority of the SMV. An upper endoscopy revealed no varices. Colonoscopy revealed large rectal varices that were felt to be too large for banding. The patient was recommended for TIPS balloon angioplasty and underwent thrombectomy with post intervention portal venous gradient of 14 mm (from 30 mmHg). However, during the procedure of balloon-occluded retrograde transvenous obliteration (BRTO), the patient developed atrial flutter and the procedure was aborted. Post procedure he developed massive hematochezia requiring transfusion. A bedside flexible sigmoidoscopy revealed large amount of rectal blood with clots, most likely bleeding from the rectal varices and precluding adequate visualization. A Sengstaken-Blakemore tube was inserted and inflated with 200mls of saline, into the rectum with complete resolution of bleeding. The balloon was left in place for about 6 hours and then removed with no further bleeding. The patient was able to undergo BRTO the following day.
Discussion: Various therapeutic interventions including endoscopic variceal ligation and percutaneous transvenous obliteration have been proposed to control significant rectal variceal bleeding. However, they may not be technically feasible with severe variceal bleeding. Under these circumstances, the use of balloon tamponade merits consideration. Although this is effective in controlling 90% of esophageal variceal hemorrhage, its use for rectal varices is not widely reported. Sengstaken-Blakemore tube can be used as a temporizing rescue therapy for rectal varices not amendable to endoscopic therapy. We advocate for the use of this device as a bridging measure for rectal hemorrhage while awaiting definite therapy, and that GI fellows should receive training in its use.
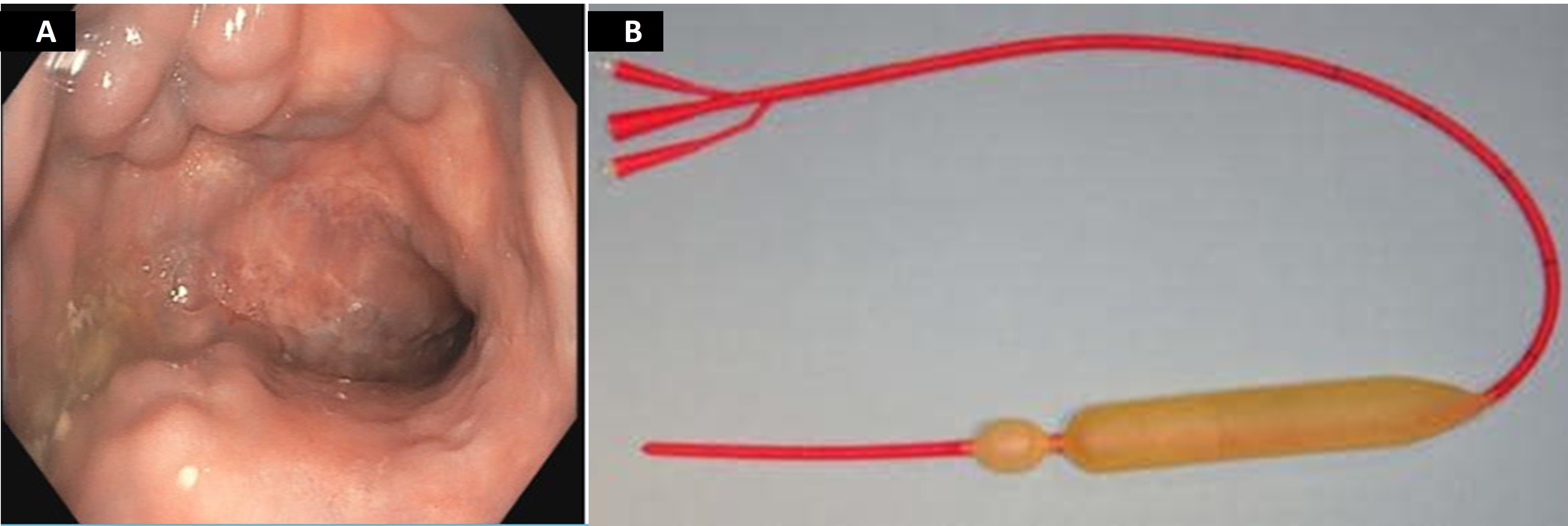
Figure: A) Large rectal varices
B) Sengstaken-Blakemore Tube ( Courtesy of google images)
B) Sengstaken-Blakemore Tube ( Courtesy of google images)
Disclosures:
Angela Barnes indicated no relevant financial relationships.
Navkiran Randhawa indicated no relevant financial relationships.
Gautam Maddineni indicated no relevant financial relationships.
Harkanwar Gill indicated no relevant financial relationships.
Satish Rao: Ironwood Pharmaceuticals – Advisory Committee/Board Member, Grant/Research Support. Pallette life sciences – Advisor or Review Panel Member.
Angela Barnes, MD, MBChB1, Navkiran Randhawa, DO1, Gautam Maddineni, MD2, Harkanwar Gill, MBBS1, Satish S. C.. Rao, MD, PhD3. P0796 - Blakemore Tamponade for Life Threatening Rectal Varices Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
