Sunday Poster Session
Category: GI Bleeding
P0802 - Rare Therapy for a Rare Condition - Successful Hemostatic Spray Treatment of Actively Bleeding Ischemic Colitis Involving the Rectum
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Scott Edelson, MD
Brooke Army Medical Center
San Antonio, TX
Presenting Author(s)
Scott Edelson, MD, Charles Miller, MD
Brooke Army Medical Center, San Antonio, TX
Introduction: Ischemic colitis (IC) is a serious condition that if not appropriately diagnosed and managed can lead to significant morbidity and mortality. IC is most often the result of sudden diminished blood flow that particularly affects the “watershed” regions of the colon, where collateral blood supply is limited. Most common affected areas are the splenic flexure and sigmoid colon. Rectal involvement is rare due to its rich collateral blood supply. We present a case of actively bleeding IC with rectal involvement in a critically ill patient, successfully treated with hemostatic spray.
Case Description/Methods: A 56 year-old male with history of severe aortic insufficiency, stroke, DM2, and CKD underwent elective aortic valve repair. This was complicated by biventricular failure requiring VA ECMO cannulation, acute renal failure requiring CRRT, ischemic hepatitis, and acute hypoxemic respiratory failure requiring continued mechanical ventilation. ECMO was complicated by prolonged hypotensive episodes requiring multiple vasoactive medications. He was also being treated for Serratia bacteremia, C. difficile, and vasopressor-induced digital ischemia.
He developed hematochezia without abdominal pain. A sigmoidoscopy revealed severely ulcerated mucosa with confluent yellowish plaques and adherent clot in the distal 25cm of the colon, consistent with ischemic colitis with rectal involvement. Diffuse oozing was noted with removal of clot, and all involved mucosa was successfully treated with hemostatic spray. Due to ongoing bleeding and worsening anemia, a repeat sigmoidoscopy 2 days later revealed clot throughout the rectum and distal sigmoid colon. After clot removal, circumferential yellowish plaques were revisualized with interspersed oozing mucosa. Again, hemostatic spray was applied with good effect. He was decannulated from VA ECMO one day after second sigmoidoscopy. No further bleeding occurred and resolution of cardiogenic shock led to progressive improvement in his condition. He was discharged to a long-term acute care hospital for recovery from his complicated hospital stay.
Discussion: Rectal involvement in nonocclusive ischemic colitis is rare, affecting only 5% of patients with IC. While hematochezia is a common symptom of IC, endoscopic treatment is not typically required for active bleeding. Few reports have described the use of hemostatic spray in IC to control bleeding. We present the safe and effective use of hemostatic spray for actively bleeding ischemic colitis involving the rectum.
Disclosures:
Scott Edelson, MD, Charles Miller, MD. P0802 - Rare Therapy for a Rare Condition - Successful Hemostatic Spray Treatment of Actively Bleeding Ischemic Colitis Involving the Rectum, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Brooke Army Medical Center, San Antonio, TX
Introduction: Ischemic colitis (IC) is a serious condition that if not appropriately diagnosed and managed can lead to significant morbidity and mortality. IC is most often the result of sudden diminished blood flow that particularly affects the “watershed” regions of the colon, where collateral blood supply is limited. Most common affected areas are the splenic flexure and sigmoid colon. Rectal involvement is rare due to its rich collateral blood supply. We present a case of actively bleeding IC with rectal involvement in a critically ill patient, successfully treated with hemostatic spray.
Case Description/Methods: A 56 year-old male with history of severe aortic insufficiency, stroke, DM2, and CKD underwent elective aortic valve repair. This was complicated by biventricular failure requiring VA ECMO cannulation, acute renal failure requiring CRRT, ischemic hepatitis, and acute hypoxemic respiratory failure requiring continued mechanical ventilation. ECMO was complicated by prolonged hypotensive episodes requiring multiple vasoactive medications. He was also being treated for Serratia bacteremia, C. difficile, and vasopressor-induced digital ischemia.
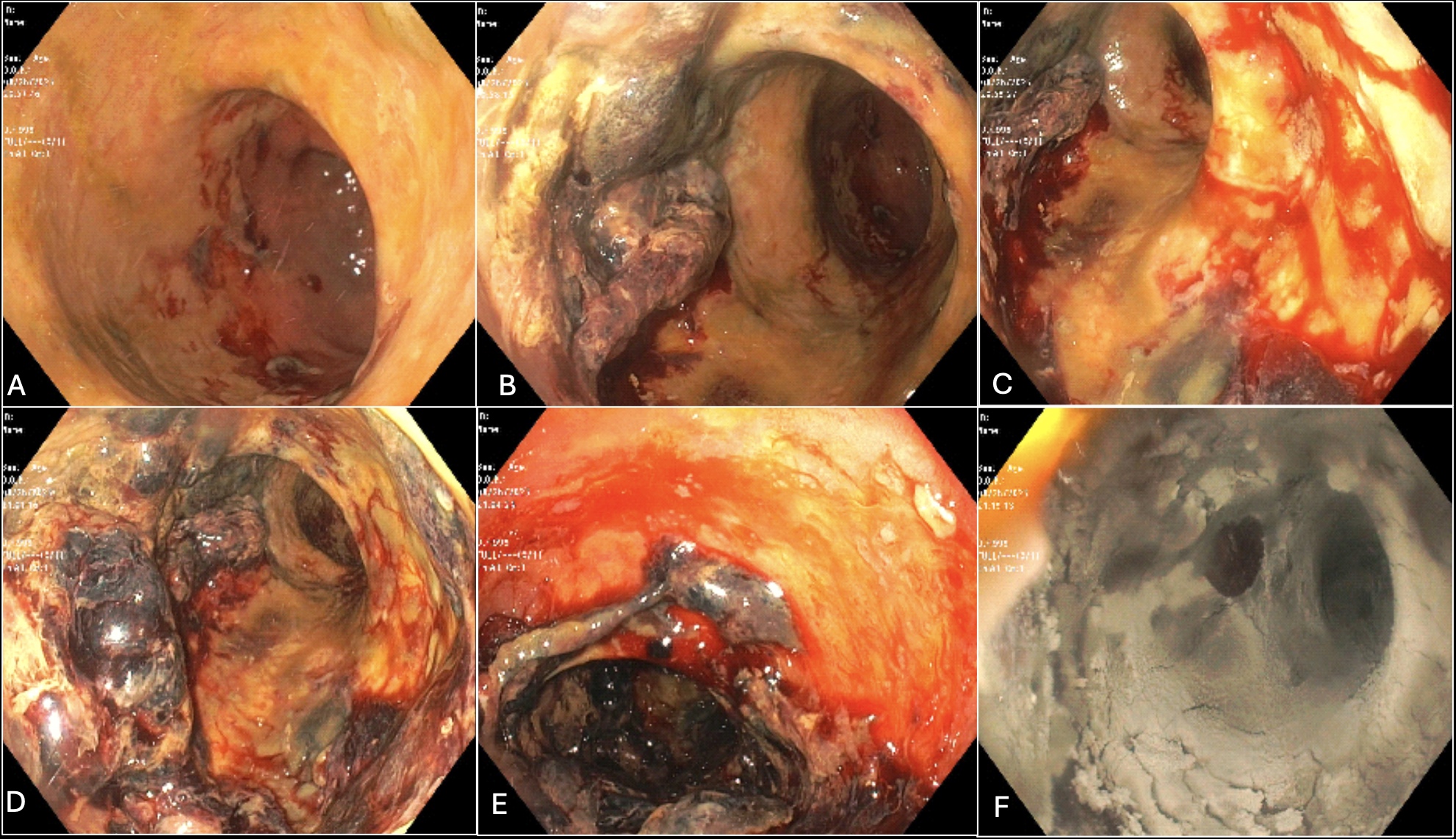
He developed hematochezia without abdominal pain. A sigmoidoscopy revealed severely ulcerated mucosa with confluent yellowish plaques and adherent clot in the distal 25cm of the colon, consistent with ischemic colitis with rectal involvement. Diffuse oozing was noted with removal of clot, and all involved mucosa was successfully treated with hemostatic spray. Due to ongoing bleeding and worsening anemia, a repeat sigmoidoscopy 2 days later revealed clot throughout the rectum and distal sigmoid colon. After clot removal, circumferential yellowish plaques were revisualized with interspersed oozing mucosa. Again, hemostatic spray was applied with good effect. He was decannulated from VA ECMO one day after second sigmoidoscopy. No further bleeding occurred and resolution of cardiogenic shock led to progressive improvement in his condition. He was discharged to a long-term acute care hospital for recovery from his complicated hospital stay.
Discussion: Rectal involvement in nonocclusive ischemic colitis is rare, affecting only 5% of patients with IC. While hematochezia is a common symptom of IC, endoscopic treatment is not typically required for active bleeding. Few reports have described the use of hemostatic spray in IC to control bleeding. We present the safe and effective use of hemostatic spray for actively bleeding ischemic colitis involving the rectum.
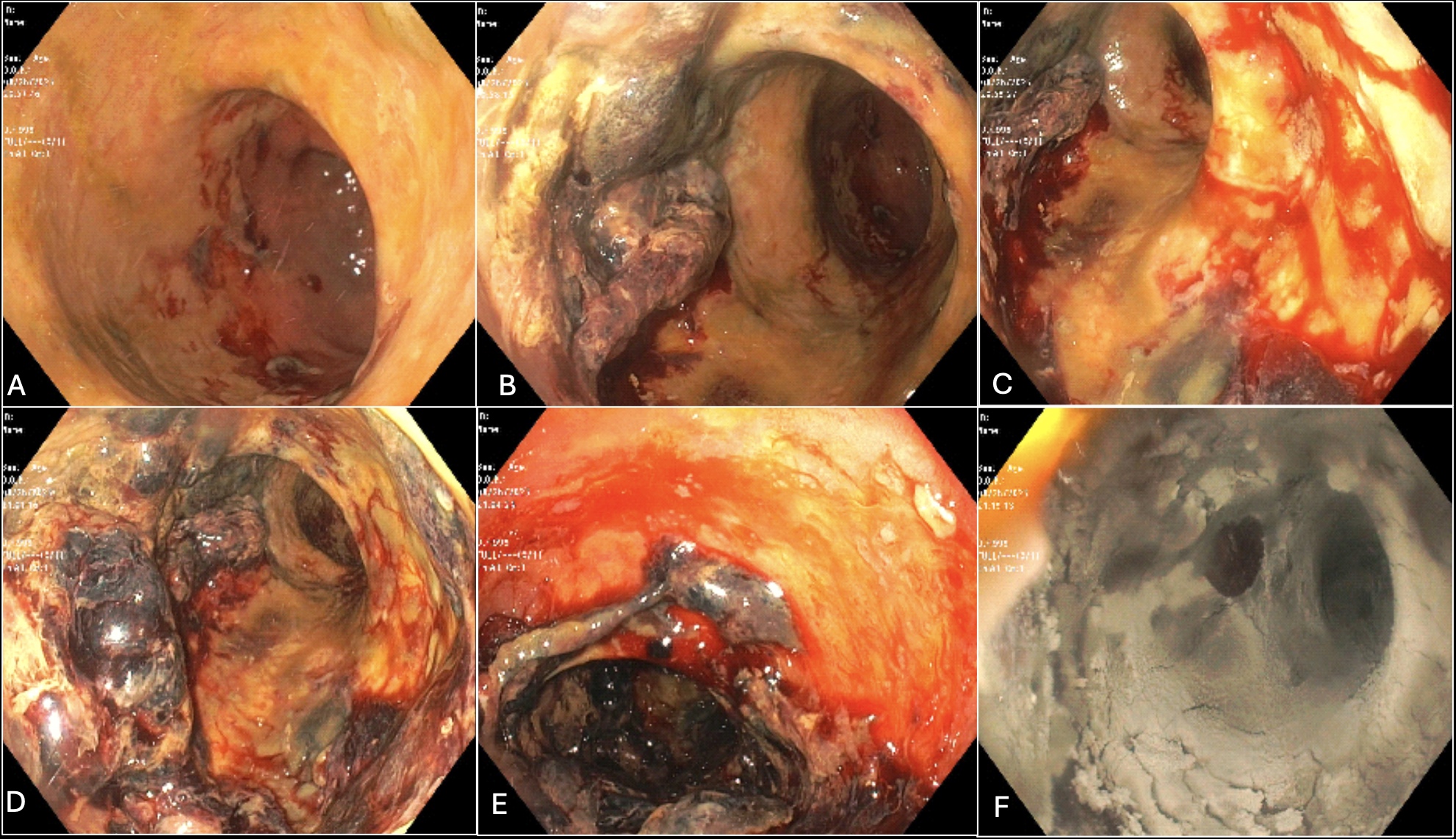
Figure: A: Ischemic colitis beginning 25cm from anal verge
B: Ischemic colitis affecting distal sigmoid colon
C: Mucosal oozing in distal sigmoid colon
D: Ischemic colitis in rectum before washing
E: Mucosal oozing in rectum after washing
F: Application of hemostatic spray to rectal wall
B: Ischemic colitis affecting distal sigmoid colon
C: Mucosal oozing in distal sigmoid colon
D: Ischemic colitis in rectum before washing
E: Mucosal oozing in rectum after washing
F: Application of hemostatic spray to rectal wall
Disclosures:
Scott Edelson indicated no relevant financial relationships.
Charles Miller indicated no relevant financial relationships.
Scott Edelson, MD, Charles Miller, MD. P0802 - Rare Therapy for a Rare Condition - Successful Hemostatic Spray Treatment of Actively Bleeding Ischemic Colitis Involving the Rectum, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
