Sunday Poster Session
Category: General Endoscopy
P0709 - The Need for Clear Endoscopic Surveillance Guidelines in Patients With Gardner Syndrome
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- DK
Daniel Kurtz, DO
Mount Sinai South Nassau, Icahn School of Medicine at Mount Sinai
Oceanside, NY
Presenting Author(s)
Daniel Kurtz, DO, Muhddesa Lakhana, DO, Pranay Srivastava, MD, Daniel Bleykhman, MD
Mount Sinai South Nassau, Icahn School of Medicine at Mount Sinai, Oceanside, NY
Introduction: Gardner Syndrome is a rare disease characterized by numerous polyps in the colon and intestines, often accompanied by osteomas, dental abnormalities, desmoid tumors, and congenital hypertrophy of the retinal pigment epithelium. It is a form of familial adenomatous polyposis (FAP) associated with a mutation in the APC gene. There is no known cure, but prophylactic total colectomy or proctocolectomy with ileal pouch-anal anastomosis (IPAA) is often performed to eliminate the risk of colon cancer. However, there are no current guidelines for endoscopic surveillance of Gardner Syndrome patients who underwent surgery. Unlike patients with ulcerative colitis (UC) who may not need surveillance post-IPAA with mucosectomy, Gardner Syndrome patients are at risk of developing polyps throughout the small intestine.
Case Description/Methods: This is a case of a 45-year-old male with Gardner Syndrome and a family history of FAP in his mother, who had a proctocolectomy with IPAA and rectal mucosectomy at age 15, and presented with a hemoglobin of 6. His Gardner Syndrome was diagnosed after he was found with an osteoma. Post-IPAA, he was told he no longer needed surveillance due to rectal mucosectomy and never had follow-up endoscopies.
EGD this hospitalization revealed a small sessile polyp in the gastric body and a large sessile mass and single sessile polyp in the duodenum. Colonoscopy showed multiple polyps in the ileal reservoir and one protruding polyp. Pathology identified the gastric polyp as a cystic fundic gland polyp, the duodenal mass as a tubular adenoma, and the ileal polyps as tubulovillous and villous adenomas. He was referred to a Familial Adenomatous Polyposis Center for a multidisciplinary approach.
Discussion: Prevention is the primary approach for Gardner Syndrome, with colonoscopies recommended for monitoring. Colectomy may be recommended if 30 or more polyps are seen. Patients with Gardner Syndrome who have not had a colectomy by age 40 are likely to develop colon cancer.
No specific endoscopic surveillance guidelines exist for FAP or Gardner Syndrome patients with IRA or IPAA. This led our patient to be managed similar to a UC patient, and thus he was was falsely assured he was no longer at risk.
Our case highlights the need for clear endoscopic surveillance guidelines to prevent morbidity and mortality in Gardner Syndrome patients, emphasizing the necessity for ongoing surveillance even after proctocolectomy with IPAA and mucosectomy due to the risk of polyposis in the small intestine.

Disclosures:
Daniel Kurtz, DO, Muhddesa Lakhana, DO, Pranay Srivastava, MD, Daniel Bleykhman, MD. P0709 - The Need for Clear Endoscopic Surveillance Guidelines in Patients With Gardner Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mount Sinai South Nassau, Icahn School of Medicine at Mount Sinai, Oceanside, NY
Introduction: Gardner Syndrome is a rare disease characterized by numerous polyps in the colon and intestines, often accompanied by osteomas, dental abnormalities, desmoid tumors, and congenital hypertrophy of the retinal pigment epithelium. It is a form of familial adenomatous polyposis (FAP) associated with a mutation in the APC gene. There is no known cure, but prophylactic total colectomy or proctocolectomy with ileal pouch-anal anastomosis (IPAA) is often performed to eliminate the risk of colon cancer. However, there are no current guidelines for endoscopic surveillance of Gardner Syndrome patients who underwent surgery. Unlike patients with ulcerative colitis (UC) who may not need surveillance post-IPAA with mucosectomy, Gardner Syndrome patients are at risk of developing polyps throughout the small intestine.
Case Description/Methods: This is a case of a 45-year-old male with Gardner Syndrome and a family history of FAP in his mother, who had a proctocolectomy with IPAA and rectal mucosectomy at age 15, and presented with a hemoglobin of 6. His Gardner Syndrome was diagnosed after he was found with an osteoma. Post-IPAA, he was told he no longer needed surveillance due to rectal mucosectomy and never had follow-up endoscopies.
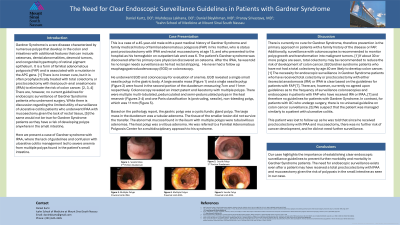
EGD this hospitalization revealed a small sessile polyp in the gastric body and a large sessile mass and single sessile polyp in the duodenum. Colonoscopy showed multiple polyps in the ileal reservoir and one protruding polyp. Pathology identified the gastric polyp as a cystic fundic gland polyp, the duodenal mass as a tubular adenoma, and the ileal polyps as tubulovillous and villous adenomas. He was referred to a Familial Adenomatous Polyposis Center for a multidisciplinary approach.
Discussion: Prevention is the primary approach for Gardner Syndrome, with colonoscopies recommended for monitoring. Colectomy may be recommended if 30 or more polyps are seen. Patients with Gardner Syndrome who have not had a colectomy by age 40 are likely to develop colon cancer.
No specific endoscopic surveillance guidelines exist for FAP or Gardner Syndrome patients with IRA or IPAA. This led our patient to be managed similar to a UC patient, and thus he was was falsely assured he was no longer at risk.
Our case highlights the need for clear endoscopic surveillance guidelines to prevent morbidity and mortality in Gardner Syndrome patients, emphasizing the necessity for ongoing surveillance even after proctocolectomy with IPAA and mucosectomy due to the risk of polyposis in the small intestine.

Figure: Ileal reservoir with multiple multi-lobulated, pedunculated and semi-pedunculated polyps
Disclosures:
Daniel Kurtz indicated no relevant financial relationships.
Muhddesa Lakhana indicated no relevant financial relationships.
Pranay Srivastava indicated no relevant financial relationships.
Daniel Bleykhman indicated no relevant financial relationships.
Daniel Kurtz, DO, Muhddesa Lakhana, DO, Pranay Srivastava, MD, Daniel Bleykhman, MD. P0709 - The Need for Clear Endoscopic Surveillance Guidelines in Patients With Gardner Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
