Sunday Poster Session
Category: General Endoscopy
P0717 - Uvular Edema and Necrosis Following Esophagogastroduodenoscopy: A Rare but Notable Complication
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- HJ
Hasan Jaber, MD
University of Kansas School of Medicine
Wichita, KS
Presenting Author(s)
Hasan Jaber, MD1, Obada Tayyem, MD2, Mahmoud Mahdi, MD1, Nader Al Souky, MD1, Gebran Khneizer, MD2
1University of Kansas School of Medicine, Wichita, KS; 2Kansas Gastroenterology and Endoscopy, LLC, Wichita, KS
Introduction: Uvular necrosis is an uncommon complication of esophagogastroduodenoscopy (EGD) and should be considered in the differential diagnosis for sore throat following the procedure. In this report, we present a case of uvular necrosis after EGD and the approach to management.
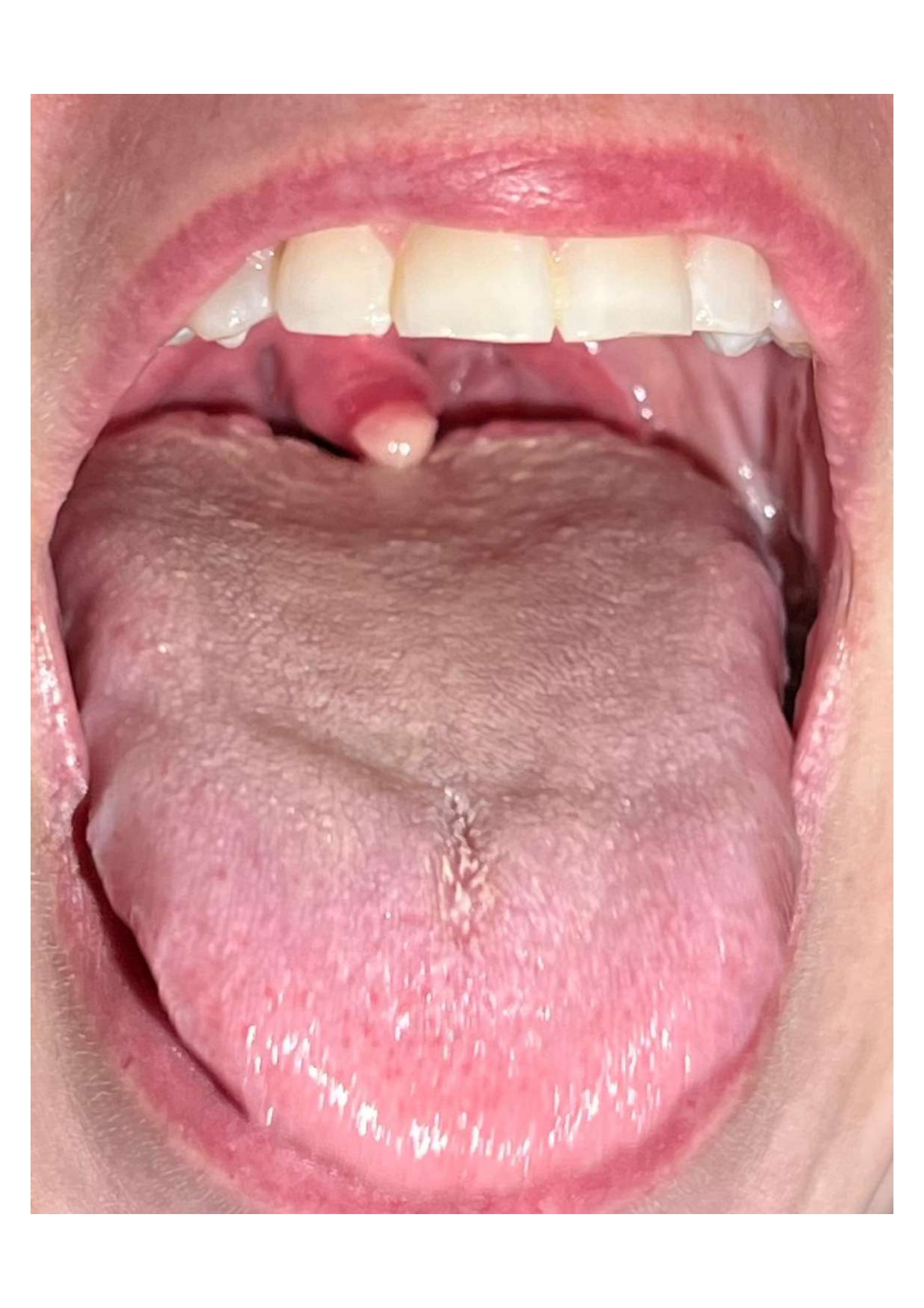
Case Description/Methods: A 40-year-old female with a history of asthma and obesity presented with complaints of dysphagia to solids and odynophagia. She denied prior episode of food impaction. An EGD was performed to evaluate her dysphagia and revealed furrows, rings and exudates of the esophagus concerning for eosinophilic esophagitis and proximal and distal esophageal biopsies were taken. The end of the procedure was complicated by hypoxia requiring mask ventilation and application of cannula suction. Her oxygen saturation returned to normal, and she was discharged home after the procedure. The following day, she returned with severe sore throat, a foreign body sensation, and odynophagia. She was asked to present to clinic and physical examination revealed uvular edema and a white exudate at the uvula’s tip which was highly suggestive of uvular edema with necrosis. She was treated with supportive care consisting of analgesics and prednisone 30 mg daily for three days. The patient began to improve the next day and was able to resume regular oral intake of food after treatment.
Discussion: Uvular necrosis is a rare complication following an EGD. While a sore throat can occur transiently post-EGD, persistent sore throat should raise suspicion for uvular necrosis. Potential causes include obstruction of the uvula's blood supply, excessive suctioning during scope withdrawal, or cannula suction trauma to the uvula. Symptoms are generally nonspecific and may include severe sore throat, dysphagia, odynophagia, and a foreign body sensation. Diagnosis is made clinically through physical examination, which typically reveals white or yellow exudate, possibly with a black tip, and uvular edema. Treatment is conservative, involving analgesics, prednisone, and rarely antibiotics if infection signs are present.
In summary, although uvular necrosis is uncommon and potentially underdiagnosed post EGD, endoscopists should be aware of this complication to ensure early detection, management, and patient education to prevent further complications.
Disclosures:
Hasan Jaber, MD1, Obada Tayyem, MD2, Mahmoud Mahdi, MD1, Nader Al Souky, MD1, Gebran Khneizer, MD2. P0717 - Uvular Edema and Necrosis Following Esophagogastroduodenoscopy: A Rare but Notable Complication, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Kansas School of Medicine, Wichita, KS; 2Kansas Gastroenterology and Endoscopy, LLC, Wichita, KS
Introduction: Uvular necrosis is an uncommon complication of esophagogastroduodenoscopy (EGD) and should be considered in the differential diagnosis for sore throat following the procedure. In this report, we present a case of uvular necrosis after EGD and the approach to management.
Case Description/Methods: A 40-year-old female with a history of asthma and obesity presented with complaints of dysphagia to solids and odynophagia. She denied prior episode of food impaction. An EGD was performed to evaluate her dysphagia and revealed furrows, rings and exudates of the esophagus concerning for eosinophilic esophagitis and proximal and distal esophageal biopsies were taken. The end of the procedure was complicated by hypoxia requiring mask ventilation and application of cannula suction. Her oxygen saturation returned to normal, and she was discharged home after the procedure. The following day, she returned with severe sore throat, a foreign body sensation, and odynophagia. She was asked to present to clinic and physical examination revealed uvular edema and a white exudate at the uvula’s tip which was highly suggestive of uvular edema with necrosis. She was treated with supportive care consisting of analgesics and prednisone 30 mg daily for three days. The patient began to improve the next day and was able to resume regular oral intake of food after treatment.
Discussion: Uvular necrosis is a rare complication following an EGD. While a sore throat can occur transiently post-EGD, persistent sore throat should raise suspicion for uvular necrosis. Potential causes include obstruction of the uvula's blood supply, excessive suctioning during scope withdrawal, or cannula suction trauma to the uvula. Symptoms are generally nonspecific and may include severe sore throat, dysphagia, odynophagia, and a foreign body sensation. Diagnosis is made clinically through physical examination, which typically reveals white or yellow exudate, possibly with a black tip, and uvular edema. Treatment is conservative, involving analgesics, prednisone, and rarely antibiotics if infection signs are present.
In summary, although uvular necrosis is uncommon and potentially underdiagnosed post EGD, endoscopists should be aware of this complication to ensure early detection, management, and patient education to prevent further complications.
Figure: Figure 1: Necrotized uvula with white exudate on day 1 after EGD
Disclosures:
Hasan Jaber indicated no relevant financial relationships.
Obada Tayyem indicated no relevant financial relationships.
Mahmoud Mahdi indicated no relevant financial relationships.
Nader Al Souky indicated no relevant financial relationships.
Gebran Khneizer indicated no relevant financial relationships.
Hasan Jaber, MD1, Obada Tayyem, MD2, Mahmoud Mahdi, MD1, Nader Al Souky, MD1, Gebran Khneizer, MD2. P0717 - Uvular Edema and Necrosis Following Esophagogastroduodenoscopy: A Rare but Notable Complication, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
