Sunday Poster Session
Category: General Endoscopy
P0722 - Symptomatic Small Bowel Obstruction Due to PEG Internal Bumper Migration to the Distal Small Intestine
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Kaitlyn Cronk, MD
University of Mississippi Medical Center
Jackson, MS
Presenting Author(s)
Kaitlyn Cronk, MD, Anna Lauren G. Winter, MD, Anna H.. Owings, DO, Shou-jiang Tang, MD
University of Mississippi Medical Center, Jackson, MS
Introduction: Percutaneous endoscopic gastrostomy (PEG) tube placement is one of the most common endoscopic procedures worldwide and is the preferred route of enteral feeding in patients with poor oral intake. Most patients do well with PEG tubes, however, they can result in minor and even major complications. Removal is recommended if the PEG tube is no longer needed. Here, we present a case of a small bowel obstruction (SBO) caused by PEG internal bumper dislodgement and migration to the distal small intestine.
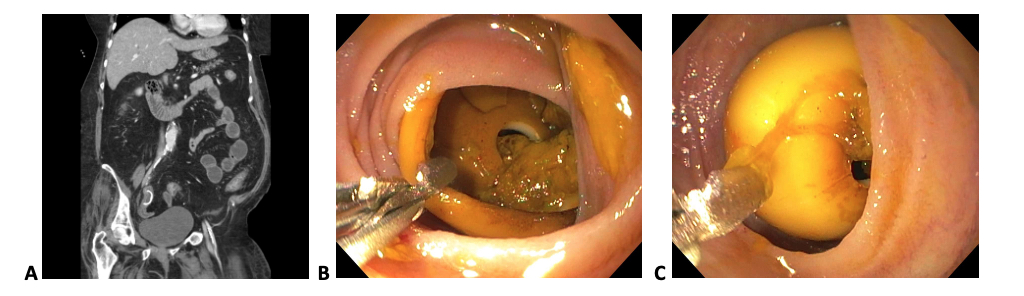
Case Description/Methods: A 62-year-old female with a history of stroke from a ruptured aneurysm, hypertension, and rheumatoid arthritis who was previously tracheostomy and PEG tube dependent presented with abdominal pain, nausea, and diarrhea for several days. The patient had not required her PEG tube for nutrition for quite some time. The PEG tube was attempted to be removed the week prior, but there was suspicion a piece was retained. Computerized tomography (CT) of the abdomen and pelvis was significant for a dislodged PEG bumper in the distal ileum concern for developing small bowel obstruction. A colonoscopy was performed for foreign body retrieval, but PEG bumperretrieval was unsuccessful. The following day a colonoscopy with a single-balloon enteroscope and retrogradeenteroscopy was performed. The distal ileum was visualized with identification of the foreign body (PEG internal bumper), which was successfully removed with a Raptor grasping device. While in post-procedure recovery, the patient aspirated and subsequently desaturated requiring intubation and transfer to the intensive care unit. These complications resulted in an almost three-month long hospitalization, and ultimately, the patient was discharged to short-term rehabilitation.
Discussion: PEG tube placement is often regarded as a more “benign” procedure due to its consideration as a common and overall low-risk procedure. However, PEG tube placement can still have serious complications. In our case, thepatient’s SBO was caused by migration of the PEG tube’s dislodged internal bumper. This was ultimately aconsequence of not removing her PEG tube when indicated and resulted in a complicated, almost 90-day hospitalization. This case highlights the importance of evaluating continued PEG tube necessity, potential complications, and patient education. As clinicians, we must be aware of complications of seemingly “benign” procedures and work to avoid them in our patients, in this case by recognizing indications for PEG tube removal.
Disclosures:
Kaitlyn Cronk, MD, Anna Lauren G. Winter, MD, Anna H.. Owings, DO, Shou-jiang Tang, MD. P0722 - Symptomatic Small Bowel Obstruction Due to PEG Internal Bumper Migration to the Distal Small Intestine, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Mississippi Medical Center, Jackson, MS
Introduction: Percutaneous endoscopic gastrostomy (PEG) tube placement is one of the most common endoscopic procedures worldwide and is the preferred route of enteral feeding in patients with poor oral intake. Most patients do well with PEG tubes, however, they can result in minor and even major complications. Removal is recommended if the PEG tube is no longer needed. Here, we present a case of a small bowel obstruction (SBO) caused by PEG internal bumper dislodgement and migration to the distal small intestine.
Case Description/Methods: A 62-year-old female with a history of stroke from a ruptured aneurysm, hypertension, and rheumatoid arthritis who was previously tracheostomy and PEG tube dependent presented with abdominal pain, nausea, and diarrhea for several days. The patient had not required her PEG tube for nutrition for quite some time. The PEG tube was attempted to be removed the week prior, but there was suspicion a piece was retained. Computerized tomography (CT) of the abdomen and pelvis was significant for a dislodged PEG bumper in the distal ileum concern for developing small bowel obstruction. A colonoscopy was performed for foreign body retrieval, but PEG bumperretrieval was unsuccessful. The following day a colonoscopy with a single-balloon enteroscope and retrogradeenteroscopy was performed. The distal ileum was visualized with identification of the foreign body (PEG internal bumper), which was successfully removed with a Raptor grasping device. While in post-procedure recovery, the patient aspirated and subsequently desaturated requiring intubation and transfer to the intensive care unit. These complications resulted in an almost three-month long hospitalization, and ultimately, the patient was discharged to short-term rehabilitation.
Discussion: PEG tube placement is often regarded as a more “benign” procedure due to its consideration as a common and overall low-risk procedure. However, PEG tube placement can still have serious complications. In our case, thepatient’s SBO was caused by migration of the PEG tube’s dislodged internal bumper. This was ultimately aconsequence of not removing her PEG tube when indicated and resulted in a complicated, almost 90-day hospitalization. This case highlights the importance of evaluating continued PEG tube necessity, potential complications, and patient education. As clinicians, we must be aware of complications of seemingly “benign” procedures and work to avoid them in our patients, in this case by recognizing indications for PEG tube removal.
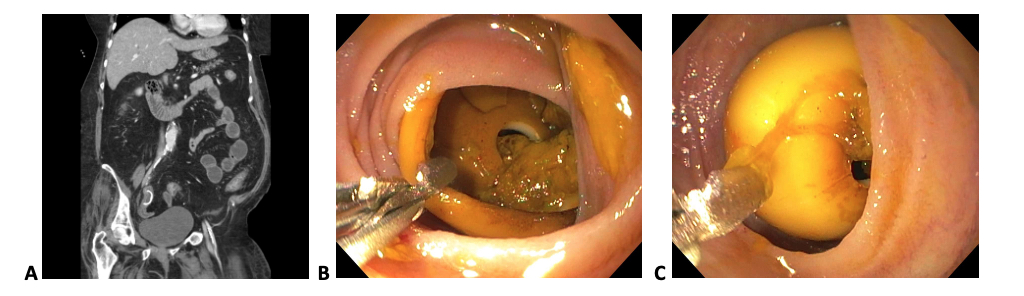
Figure: A. CT concerning for SBO with dislodged PEG bumper.
B. Foreign body (PEG internal bumper) in the distal ileum.
C. Successful removal of PEG internal bumper with Raptor grasping device.
B. Foreign body (PEG internal bumper) in the distal ileum.
C. Successful removal of PEG internal bumper with Raptor grasping device.
Disclosures:
Kaitlyn Cronk indicated no relevant financial relationships.
Anna Lauren Winter indicated no relevant financial relationships.
Anna Owings indicated no relevant financial relationships.
Shou-jiang Tang indicated no relevant financial relationships.
Kaitlyn Cronk, MD, Anna Lauren G. Winter, MD, Anna H.. Owings, DO, Shou-jiang Tang, MD. P0722 - Symptomatic Small Bowel Obstruction Due to PEG Internal Bumper Migration to the Distal Small Intestine, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
