Sunday Poster Session
Category: Esophagus
P0579 - Black Esophagus Unveiled: Insights Into Acute Esophageal Necrosis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
Ammar Hasan, MD
HCA Kingwood
Kingwood, TX
Presenting Author(s)
Ammar Hasan, MD1, Nouman Shafique, MD2, Asad Rehman, DO1, Mahnoor Hashmi, MD1, Bushra Bangash, MD1, Ismail Hader, MD1
1HCA Kingwood, Kingwood, TX; 2AdventHealth Medical Group, AdventHealth, Orlando, FL
Introduction: Acute esophageal necrosis (AEN), colloquially known as black esophagus, is a rare and life-threatening condition characterized by circumferential blackening of the esophagus. It predominantly afflicts individuals aged 60 to 80 and is often associated with significant medical comorbidities. AEN typically results from a combination of ischemia and a topical insult to the esophagus in severely sick patients. Despite its rarity, prompt recognition and comprehensive management are crucial in optimizing patient outcomes.
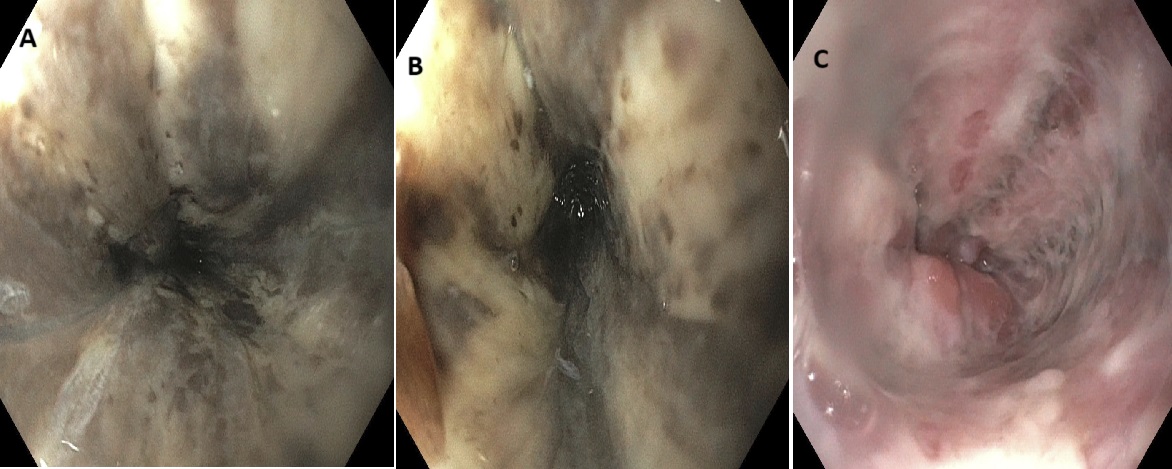
Case Description/Methods: A 36-year-old male with a past medical history of alcohol abuse and insulin-dependent diabetes presented with altered mental status, multiple episodes of seizure-like activity, and hematemesis. Upon initial assessment, the Patient was found to be hypotensive and having ventricular tachycardia for which the patient was successfully cardioverted. Subsequently, the patient was intubated for airway protection. Initial work-up revealed a pH of 7.11, blood glucose of 599, Creatine kinase (CK) 20931, Potassium 7.9, and lactic acid of 5.3. The patient was treated for multiple acute medical problems including diabetic ketoacidosis (DKA), acute pancreatitis, acute kidney injury (AKI) with rhabdomyolysis, severe hyperkalemia, and seizure disorder. The patient was admitted to the ICU and emergent hemodialysis was initiated. CT abdomen/pelvis was unremarkable on admission and the patient subsequently underwent EGD due to concerns for upper gastrointestinal (GI) bleeding which revealed LA Grade D erosive esophagitis and black esophagus (Figures A and B) concerning for acute esophageal necrosis. Management involved supportive care and addressing the underlying acute conditions. One week later, a repeat EGD showed healing esophageal mucosa (Figure C).
Discussion: This case underscores the challenge of managing AEN in a young patient with significant medical comorbidities. The interplay of acute ischemia, metabolic derangements, and potential infectious insult underscores the complexity of the condition. Multidisciplinary collaboration was pivotal in stabilizing the patient and mitigating further complications. Prompt recognition and comprehensive treatment were essential in this critical scenario. While AEN is rare, its consideration in patients with GI bleeding and systemic illness is paramount. Further research is warranted to optimize diagnostic and therapeutic strategies, enhancing patient outcomes in such challenging cases.
Disclosures:
Ammar Hasan, MD1, Nouman Shafique, MD2, Asad Rehman, DO1, Mahnoor Hashmi, MD1, Bushra Bangash, MD1, Ismail Hader, MD1. P0579 - Black Esophagus Unveiled: Insights Into Acute Esophageal Necrosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1HCA Kingwood, Kingwood, TX; 2AdventHealth Medical Group, AdventHealth, Orlando, FL
Introduction: Acute esophageal necrosis (AEN), colloquially known as black esophagus, is a rare and life-threatening condition characterized by circumferential blackening of the esophagus. It predominantly afflicts individuals aged 60 to 80 and is often associated with significant medical comorbidities. AEN typically results from a combination of ischemia and a topical insult to the esophagus in severely sick patients. Despite its rarity, prompt recognition and comprehensive management are crucial in optimizing patient outcomes.
Case Description/Methods: A 36-year-old male with a past medical history of alcohol abuse and insulin-dependent diabetes presented with altered mental status, multiple episodes of seizure-like activity, and hematemesis. Upon initial assessment, the Patient was found to be hypotensive and having ventricular tachycardia for which the patient was successfully cardioverted. Subsequently, the patient was intubated for airway protection. Initial work-up revealed a pH of 7.11, blood glucose of 599, Creatine kinase (CK) 20931, Potassium 7.9, and lactic acid of 5.3. The patient was treated for multiple acute medical problems including diabetic ketoacidosis (DKA), acute pancreatitis, acute kidney injury (AKI) with rhabdomyolysis, severe hyperkalemia, and seizure disorder. The patient was admitted to the ICU and emergent hemodialysis was initiated. CT abdomen/pelvis was unremarkable on admission and the patient subsequently underwent EGD due to concerns for upper gastrointestinal (GI) bleeding which revealed LA Grade D erosive esophagitis and black esophagus (Figures A and B) concerning for acute esophageal necrosis. Management involved supportive care and addressing the underlying acute conditions. One week later, a repeat EGD showed healing esophageal mucosa (Figure C).
Discussion: This case underscores the challenge of managing AEN in a young patient with significant medical comorbidities. The interplay of acute ischemia, metabolic derangements, and potential infectious insult underscores the complexity of the condition. Multidisciplinary collaboration was pivotal in stabilizing the patient and mitigating further complications. Prompt recognition and comprehensive treatment were essential in this critical scenario. While AEN is rare, its consideration in patients with GI bleeding and systemic illness is paramount. Further research is warranted to optimize diagnostic and therapeutic strategies, enhancing patient outcomes in such challenging cases.
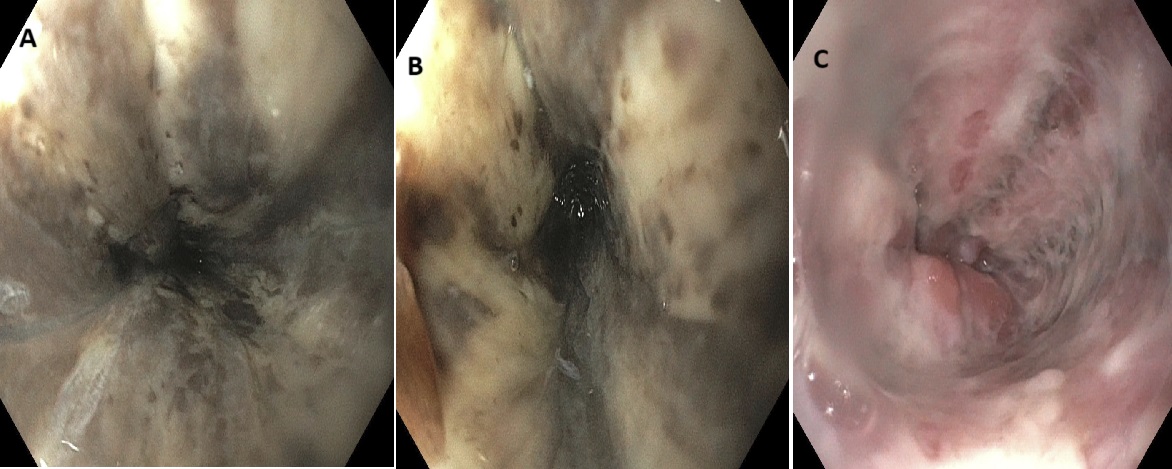
Figure: Figures A and B indicate black esophagus.
Disclosures:
Ammar Hasan indicated no relevant financial relationships.
Nouman Shafique indicated no relevant financial relationships.
Asad Rehman indicated no relevant financial relationships.
Mahnoor Hashmi indicated no relevant financial relationships.
Bushra Bangash indicated no relevant financial relationships.
Ismail Hader indicated no relevant financial relationships.
Ammar Hasan, MD1, Nouman Shafique, MD2, Asad Rehman, DO1, Mahnoor Hashmi, MD1, Bushra Bangash, MD1, Ismail Hader, MD1. P0579 - Black Esophagus Unveiled: Insights Into Acute Esophageal Necrosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
