Sunday Poster Session
Category: Esophagus
P0581 - A Novel Approach for Managing Blown Out Myotomy After POEM or Heller Myotomy Using Endoscopic Bands
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpeg.jpg)
Arsh Momin, MD
Penn State Health Milton S. Hershey Medical Center
Atlanta, GA
Presenting Author(s)
Award: Presidential Poster Award
Arsh Momin, MD1, Vinayak Shenoy, DO2, Abraham Mathew, MD2
1Penn State Health Milton S. Hershey Medical Center, Atlanta, GA; 2Penn State Health Milton S. Hershey Medical Center, Hershey, PA
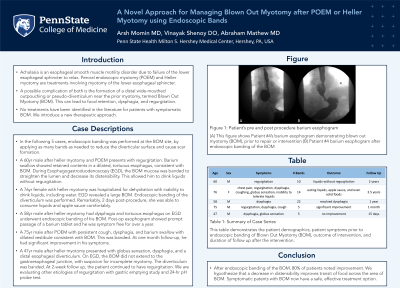
Introduction: Achalasia is an esophageal smooth muscle motility disorder due to failure of the lower esophageal sphincter to relax. Peroral endoscopic myotomy (POEM) and Heller myotomy are treatments involving myotomy of the lower esophageal sphincter. A possible complication of both is the formation of a distal wide-mouthed outpouching or pseudo-diverticulum near the prior myotomy, termed Blown Out Myotomy (BOM). This can lead to food retention, dysphagia, and regurgitation. No treatments have been identified in the literature for patients with symptomatic BOM. We introduce a new therapeutic approach.
Case Description/Methods: In the following 5 cases, endoscopic banding was performed at the BOM site, by applying as many bands as needed to reduce the diverticular surface and cause scar formation.
A 60yr male after heller myotomy and POEM presents with regurgitation. Barium swallow showed retained contents in a dilated, tortuous esophagus, consistent with BOM. During Esophagogastroduodenoscopy (EGD), the BOM mucosa was banded to straighten the lumen and decrease its distensibility. This allowed him to drink liquids without regurgitation.
A 76yr female with heller myotomy was hospitalized for dehydration with inability to drink liquids, including water. EGD revealed a large BOM. Endoscopic banding of the diverticulum was performed. Remarkably, 2 days post-procedure, she was able to consume liquids and apple sauce comfortably.
A 58yr male after heller myotomy had dysphagia and tortuous esophagus on EGD underwent endoscopic banding of his BOM. Post-op esophogram showed prompt passage of a barium tablet and he was symptom free for over a year.
A 75yr male after POEM with persistent cough, dysphagia, and barium swallow with dilated vestibule consistent with BOM. This was banded. At one month follow-up, he had significant improvement in his symptoms.
A 47yr male after heller myotomy presented with globus sensation, dysphagia, and a distal esophageal diverticulum. On EGD, the BOM did not extend to the gastroesophageal junction, with suspicion for incomplete myotomy. The diverticulum was banded. At 2-week follow up, the patient continued to have regurgitation. We are evaluating other etiologies of regurgitation with gastric emptying study and 24-hr pH probe test.
Discussion: After endoscopic banding of the BOM, 80% of patients noted improvement. We hypothesize that a decrease in distensibility improves transit of food across the area of BOM. Symptomatic patents with BOM now have a safe, effective treatment option.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Arsh Momin, MD1, Vinayak Shenoy, DO2, Abraham Mathew, MD2. P0581 - A Novel Approach for Managing Blown Out Myotomy After POEM or Heller Myotomy Using Endoscopic Bands, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Arsh Momin, MD1, Vinayak Shenoy, DO2, Abraham Mathew, MD2
1Penn State Health Milton S. Hershey Medical Center, Atlanta, GA; 2Penn State Health Milton S. Hershey Medical Center, Hershey, PA
Introduction: Achalasia is an esophageal smooth muscle motility disorder due to failure of the lower esophageal sphincter to relax. Peroral endoscopic myotomy (POEM) and Heller myotomy are treatments involving myotomy of the lower esophageal sphincter. A possible complication of both is the formation of a distal wide-mouthed outpouching or pseudo-diverticulum near the prior myotomy, termed Blown Out Myotomy (BOM). This can lead to food retention, dysphagia, and regurgitation. No treatments have been identified in the literature for patients with symptomatic BOM. We introduce a new therapeutic approach.
Case Description/Methods: In the following 5 cases, endoscopic banding was performed at the BOM site, by applying as many bands as needed to reduce the diverticular surface and cause scar formation.
A 60yr male after heller myotomy and POEM presents with regurgitation. Barium swallow showed retained contents in a dilated, tortuous esophagus, consistent with BOM. During Esophagogastroduodenoscopy (EGD), the BOM mucosa was banded to straighten the lumen and decrease its distensibility. This allowed him to drink liquids without regurgitation.
A 76yr female with heller myotomy was hospitalized for dehydration with inability to drink liquids, including water. EGD revealed a large BOM. Endoscopic banding of the diverticulum was performed. Remarkably, 2 days post-procedure, she was able to consume liquids and apple sauce comfortably.
A 58yr male after heller myotomy had dysphagia and tortuous esophagus on EGD underwent endoscopic banding of his BOM. Post-op esophogram showed prompt passage of a barium tablet and he was symptom free for over a year.
A 75yr male after POEM with persistent cough, dysphagia, and barium swallow with dilated vestibule consistent with BOM. This was banded. At one month follow-up, he had significant improvement in his symptoms.
A 47yr male after heller myotomy presented with globus sensation, dysphagia, and a distal esophageal diverticulum. On EGD, the BOM did not extend to the gastroesophageal junction, with suspicion for incomplete myotomy. The diverticulum was banded. At 2-week follow up, the patient continued to have regurgitation. We are evaluating other etiologies of regurgitation with gastric emptying study and 24-hr pH probe test.
Discussion: After endoscopic banding of the BOM, 80% of patients noted improvement. We hypothesize that a decrease in distensibility improves transit of food across the area of BOM. Symptomatic patents with BOM now have a safe, effective treatment option.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Arsh Momin indicated no relevant financial relationships.
Vinayak Shenoy indicated no relevant financial relationships.
Abraham Mathew indicated no relevant financial relationships.
Arsh Momin, MD1, Vinayak Shenoy, DO2, Abraham Mathew, MD2. P0581 - A Novel Approach for Managing Blown Out Myotomy After POEM or Heller Myotomy Using Endoscopic Bands, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

