Sunday Poster Session
Category: Esophagus
P0582 - A Second Look on Long Standing Achalasia: A Case Report of Underlying Malignancy
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Grecia M. Santaella Mendez, MD
Loma Linda University Medical Center
Redlands, CA
Presenting Author(s)
Grecia M. Santaella Mendez, MD1, Devika Gandhi, MD1, Shae Patel, DO2, Nikhil Thiruvengadam, MD3
1Loma Linda University Medical Center, Redlands, CA; 2Loma Linda University, Placentia, CA; 3Loma Linda University, Loma Linda, CA
Introduction: Achalasia is an esophageal dysmotility disorder that causes impaired lower esophageal sphincter (LES) relaxation as a result of degeneration of the nerve fibers to the LES, causing dysphagia in patients. Achalasia patients are thought to have a significantly higher risk for esophageal squamous cell cancer (SCC) as chronic inflammation leads to dysplasia and cancer, but SCC remains rare in achalasia patients.
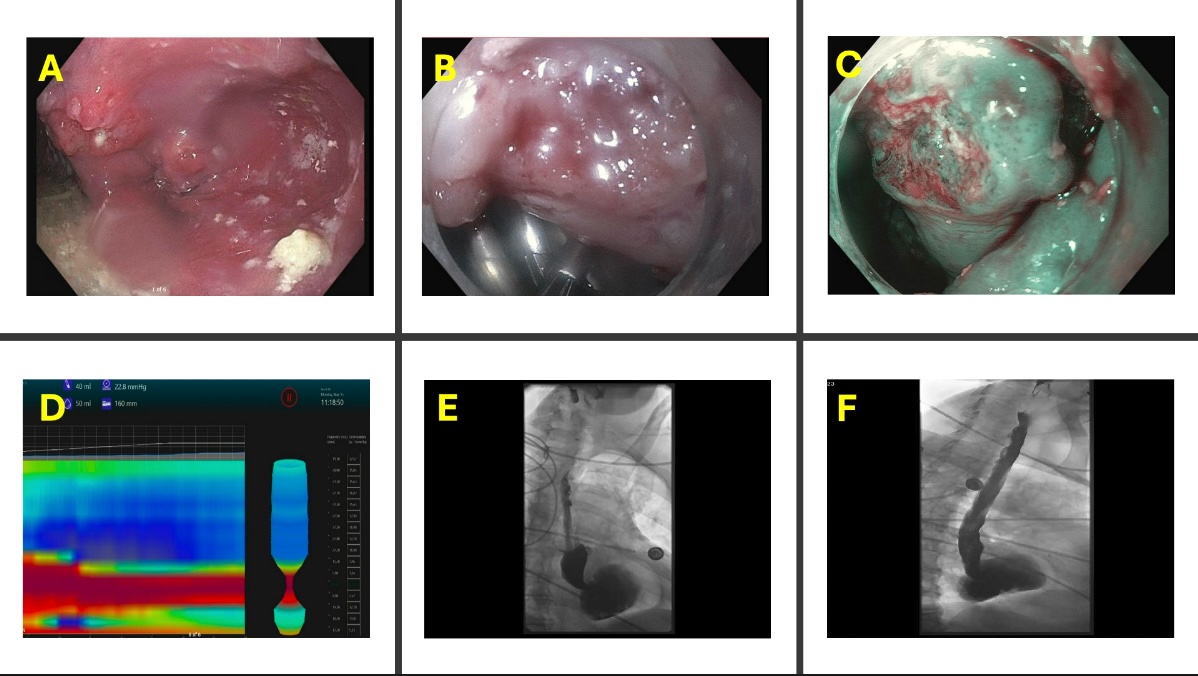
Case Description/Methods: This is the case of a 71-year-old male with previous medical diagnoses of CAD, obesity, OSA, BPH, esophageal diverticulum, idiopathic subglottic stenosis requiring recurrent tracheal dilations, and type I achalasia. The patient had undergone multiple upper endoscopies with dilation in the past for symptomatic relief. He presented to the hospital with 2-month history of progressively worsening dysphagia symptoms resulted in intolerance of solids and liquids and associated 25lb weight loss. CT chest was remarkable for a dilated and debris-filled esophagus with distal narrowing. A barium esophagogram showed a dilated esophagus with uncoordinated contractions and no contrast passage into the stomach.
Initial EGD was remarkable for findings of esophagogastric junction outlet obstruction with a large 10 cm diverticulum in the distal esophagus, the latter likely due to long-standing hyperpressurization of the esophagus. A CT Chest was performed to exclude pseudoachalasia, and no esophageal mass was noted. During repeat EGD patient was noted with recurrent food debris blockage and a large lateral diverticulum at the LES. The LES was unable to be traversed with the adult upper endoscope. The initial plan was for POEM; however, an erythematous and friable mass was identified despite difficult visualization in the setting of extensive stasis esophagitis. This was biopsied and was later confirmed to be squamous cell carcinoma (SCC). The patient underwent PEG placement and later started chemoradiation therapy.
Discussion: Achalasia management is intended to alleviate the patient’s obstructive symptoms. Surgical and nonsurgical interventions are options; however, before deciding on final management, it’s important to exclude esophageal SCC, which can develop in patients with long-standing achalasia. In our patient’s case, the decision was made to proceed with perioral endoscopic myotomy (POEM). Still, as highlighted in this case, performing an extensive and high-quality endoscopic evaluation is imperative before considering POEM.
Disclosures:
Grecia M. Santaella Mendez, MD1, Devika Gandhi, MD1, Shae Patel, DO2, Nikhil Thiruvengadam, MD3. P0582 - A Second Look on Long Standing Achalasia: A Case Report of Underlying Malignancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Loma Linda University Medical Center, Redlands, CA; 2Loma Linda University, Placentia, CA; 3Loma Linda University, Loma Linda, CA
Introduction: Achalasia is an esophageal dysmotility disorder that causes impaired lower esophageal sphincter (LES) relaxation as a result of degeneration of the nerve fibers to the LES, causing dysphagia in patients. Achalasia patients are thought to have a significantly higher risk for esophageal squamous cell cancer (SCC) as chronic inflammation leads to dysplasia and cancer, but SCC remains rare in achalasia patients.
Case Description/Methods: This is the case of a 71-year-old male with previous medical diagnoses of CAD, obesity, OSA, BPH, esophageal diverticulum, idiopathic subglottic stenosis requiring recurrent tracheal dilations, and type I achalasia. The patient had undergone multiple upper endoscopies with dilation in the past for symptomatic relief. He presented to the hospital with 2-month history of progressively worsening dysphagia symptoms resulted in intolerance of solids and liquids and associated 25lb weight loss. CT chest was remarkable for a dilated and debris-filled esophagus with distal narrowing. A barium esophagogram showed a dilated esophagus with uncoordinated contractions and no contrast passage into the stomach.
Initial EGD was remarkable for findings of esophagogastric junction outlet obstruction with a large 10 cm diverticulum in the distal esophagus, the latter likely due to long-standing hyperpressurization of the esophagus. A CT Chest was performed to exclude pseudoachalasia, and no esophageal mass was noted. During repeat EGD patient was noted with recurrent food debris blockage and a large lateral diverticulum at the LES. The LES was unable to be traversed with the adult upper endoscope. The initial plan was for POEM; however, an erythematous and friable mass was identified despite difficult visualization in the setting of extensive stasis esophagitis. This was biopsied and was later confirmed to be squamous cell carcinoma (SCC). The patient underwent PEG placement and later started chemoradiation therapy.
Discussion: Achalasia management is intended to alleviate the patient’s obstructive symptoms. Surgical and nonsurgical interventions are options; however, before deciding on final management, it’s important to exclude esophageal SCC, which can develop in patients with long-standing achalasia. In our patient’s case, the decision was made to proceed with perioral endoscopic myotomy (POEM). Still, as highlighted in this case, performing an extensive and high-quality endoscopic evaluation is imperative before considering POEM.
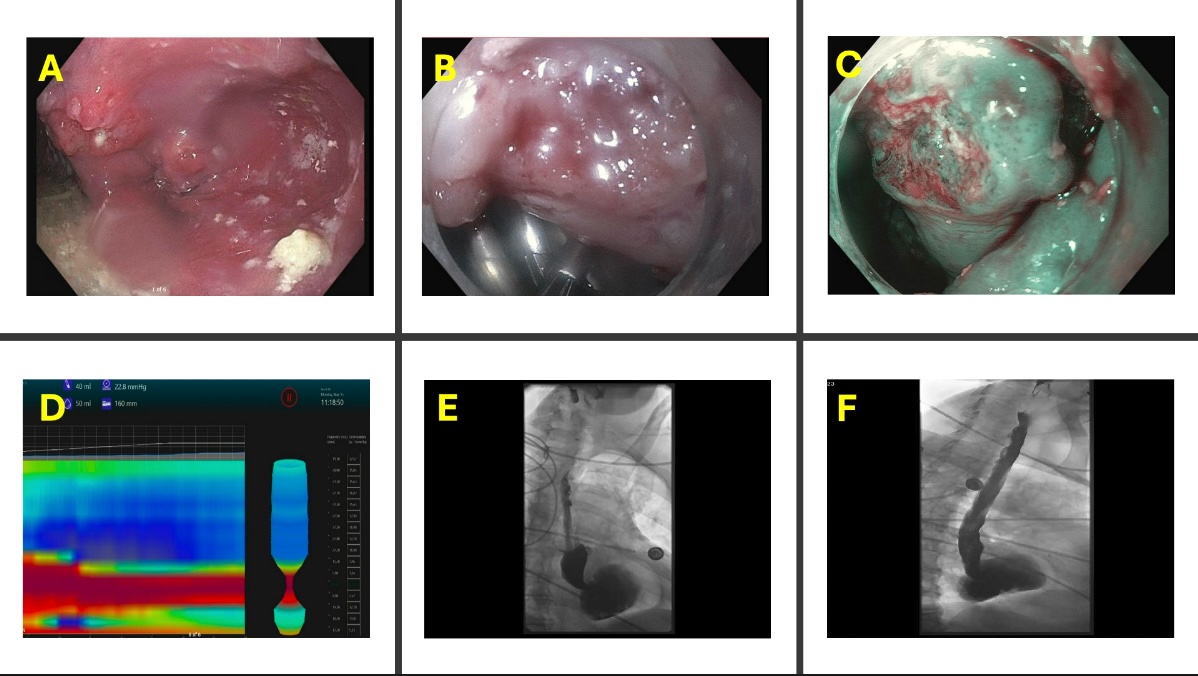
Figure: A: Initial EGD remarkable for esophagogastric outlet obstruction
B: Suspicious mucosa noted endoscopically
C: Narrow band imaging of erythematous friable mass, later confirmed to be squamous cell carcinoma
D: EndoFlip Impedance Planimetry during initial EGD suggestive of EGJOO.
E: Esophagram remarkable for contrast retention
F: Esophagram with noted esophageal distension
B: Suspicious mucosa noted endoscopically
C: Narrow band imaging of erythematous friable mass, later confirmed to be squamous cell carcinoma
D: EndoFlip Impedance Planimetry during initial EGD suggestive of EGJOO.
E: Esophagram remarkable for contrast retention
F: Esophagram with noted esophageal distension
Disclosures:
Grecia Santaella Mendez indicated no relevant financial relationships.
Devika Gandhi indicated no relevant financial relationships.
Shae Patel indicated no relevant financial relationships.
Nikhil Thiruvengadam indicated no relevant financial relationships.
Grecia M. Santaella Mendez, MD1, Devika Gandhi, MD1, Shae Patel, DO2, Nikhil Thiruvengadam, MD3. P0582 - A Second Look on Long Standing Achalasia: A Case Report of Underlying Malignancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
