Sunday Poster Session
Category: Esophagus
P0584 - When the GI Tract Takes a Detour: Colonic Interposition in Crohn's Disease
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- KT
Kimberly Tena Diaz, DO
Cooper University Hospital
Camden, NJ
Presenting Author(s)
Kimberly Tena Diaz, DO1, Andrew Alabd, MD1, Tommy Nguyen, DO2, Jay Patel, MD1, Krysta Contino, MD3
1Cooper University Hospital, Camden, NJ; 2Cooper University Hospital, Philadelphia, PA; 3Digestive Health Institute at Cooper University Hospital, Mount Laurel, NJ
Introduction: Esophageal adenocarcinoma (EAC) has rapidly become more common in Western countries. Treatment depends on the stage of mucosal invasion. Esophagectomy remains the main treatment for early-stage malignancy. Typically, a gastric conduit is preferred; however, when a gastric conduit has failed or cannot be used, the colon has been accepted as an alternative for esophageal replacement. In general, inflammatory bowel disease (IBD) is a contraindication to this surgery under planned circumstances considering potential complications of fistula, flare, and malignancy.
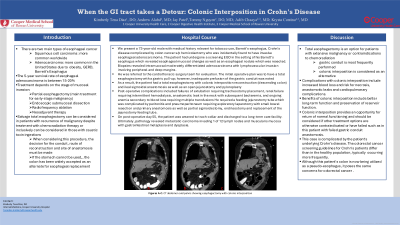
Case Description/Methods: We present a 73-year-old male with a history Barrett’s esophagus, Crohn’s disease (CD) well controlled on vedolizumab, prior history of colon cancer s/p hemicolectomy, found to have T1bN0M0 EAC with no metastatic disease on staging. He underwent a total esophagectomy, but intraoperatively, the gastric conduit was found to have inadequate perfusion given lack of blood flow in the right gastroepiploic artery. The decision was made to proceed with colonic interposition and supercharging of the graft, open jejunostomy, pyloroplasty, and splenectomy. Ultimately, pathology revealed metastatic carcinoma invading 1 of 12 lymph nodes. Post-operative course was complicated by ventilator-dependent respiratory failure, renal failure, anastomotic leak with bacteremia, and peritonitis requiring exploratory laparotomy with small bowel resection, partial sigmoidectomy and end ileostomy. It was recommended that his vedolizumab be held in the immediate post-operative period. After a long hospitalization, the patient was discharged to a long-term care facility.
Discussion: This patient with EAC and known CD maintained on biologic therapy underwent esophagectomy which was complicated by compromised gastric conduit perfusion requiring colonic interposition. This surgery can provide an opportunity for return of normal functioning and can be considered if other treatment options are otherwise contraindicated. Research studies have suggested that postoperative resumption of biologic therapy does not increase risk for intra-abdominal infections or complications related to sepsis. However, little is known about treatment, surveillance recommendations, and management of inflammatory bowel disease complications or flares for individuals with colonic interposition as it is not a commonly performed procedure. We suggest holding biologic treatment in the immediate post-operative period and continuing with routine surveillance of the graft.
Disclosures:
Kimberly Tena Diaz, DO1, Andrew Alabd, MD1, Tommy Nguyen, DO2, Jay Patel, MD1, Krysta Contino, MD3. P0584 - When the GI Tract Takes a Detour: Colonic Interposition in Crohn's Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cooper University Hospital, Camden, NJ; 2Cooper University Hospital, Philadelphia, PA; 3Digestive Health Institute at Cooper University Hospital, Mount Laurel, NJ
Introduction: Esophageal adenocarcinoma (EAC) has rapidly become more common in Western countries. Treatment depends on the stage of mucosal invasion. Esophagectomy remains the main treatment for early-stage malignancy. Typically, a gastric conduit is preferred; however, when a gastric conduit has failed or cannot be used, the colon has been accepted as an alternative for esophageal replacement. In general, inflammatory bowel disease (IBD) is a contraindication to this surgery under planned circumstances considering potential complications of fistula, flare, and malignancy.
Case Description/Methods: We present a 73-year-old male with a history Barrett’s esophagus, Crohn’s disease (CD) well controlled on vedolizumab, prior history of colon cancer s/p hemicolectomy, found to have T1bN0M0 EAC with no metastatic disease on staging. He underwent a total esophagectomy, but intraoperatively, the gastric conduit was found to have inadequate perfusion given lack of blood flow in the right gastroepiploic artery. The decision was made to proceed with colonic interposition and supercharging of the graft, open jejunostomy, pyloroplasty, and splenectomy. Ultimately, pathology revealed metastatic carcinoma invading 1 of 12 lymph nodes. Post-operative course was complicated by ventilator-dependent respiratory failure, renal failure, anastomotic leak with bacteremia, and peritonitis requiring exploratory laparotomy with small bowel resection, partial sigmoidectomy and end ileostomy. It was recommended that his vedolizumab be held in the immediate post-operative period. After a long hospitalization, the patient was discharged to a long-term care facility.
Discussion: This patient with EAC and known CD maintained on biologic therapy underwent esophagectomy which was complicated by compromised gastric conduit perfusion requiring colonic interposition. This surgery can provide an opportunity for return of normal functioning and can be considered if other treatment options are otherwise contraindicated. Research studies have suggested that postoperative resumption of biologic therapy does not increase risk for intra-abdominal infections or complications related to sepsis. However, little is known about treatment, surveillance recommendations, and management of inflammatory bowel disease complications or flares for individuals with colonic interposition as it is not a commonly performed procedure. We suggest holding biologic treatment in the immediate post-operative period and continuing with routine surveillance of the graft.
Disclosures:
Kimberly Tena Diaz indicated no relevant financial relationships.
Andrew Alabd indicated no relevant financial relationships.
Tommy Nguyen indicated no relevant financial relationships.
Jay Patel indicated no relevant financial relationships.
Krysta Contino indicated no relevant financial relationships.
Kimberly Tena Diaz, DO1, Andrew Alabd, MD1, Tommy Nguyen, DO2, Jay Patel, MD1, Krysta Contino, MD3. P0584 - When the GI Tract Takes a Detour: Colonic Interposition in Crohn's Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
