Sunday Poster Session
Category: Esophagus
P0585 - Achalasia's Tight Chokehold on Breath and Life! A Case of Severe, Compressive Achalasia Causing Acute Respiratory Failure
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Kazi T. Haque, MD
University of Texas Health, McGovern Medical School
Pearland, TX
Presenting Author(s)
Rohan Patil, BS1, Jacob Pierce. Reitnauer, BS1, Kazi T. Haque, MD2, Patrick Boddie, MD3, Fernando Sosa, BS1, Sean Ngo, BS1, Rohan Ahuja, MD1, Iyad Al-bustami, MD, MPH(c)4, Ruth Bell, DO5, Kevin K. Yu, MD1, Andrew Dupont, MD, MSPH5
1University of Texas Health, McGovern Medical School, Houston, TX; 2University of Texas Health, McGovern Medical School, Pearland, TX; 3Baylor College of Medicine, Houston, TX; 4Brooklyn Hospital Center, Houston, TX; 5McGovern Medical School at UTHealth, Houston, TX
Introduction: Achalasia is characterized by progressive esophageal dysmotility resulting in the incomplete relaxation of the lower esophageal sphincter (LES) and dysfunctional peristalsis. We present a patient who developed respiratory failure requiring endotracheal intubation due to massive food impaction secondary to severe achalasia.
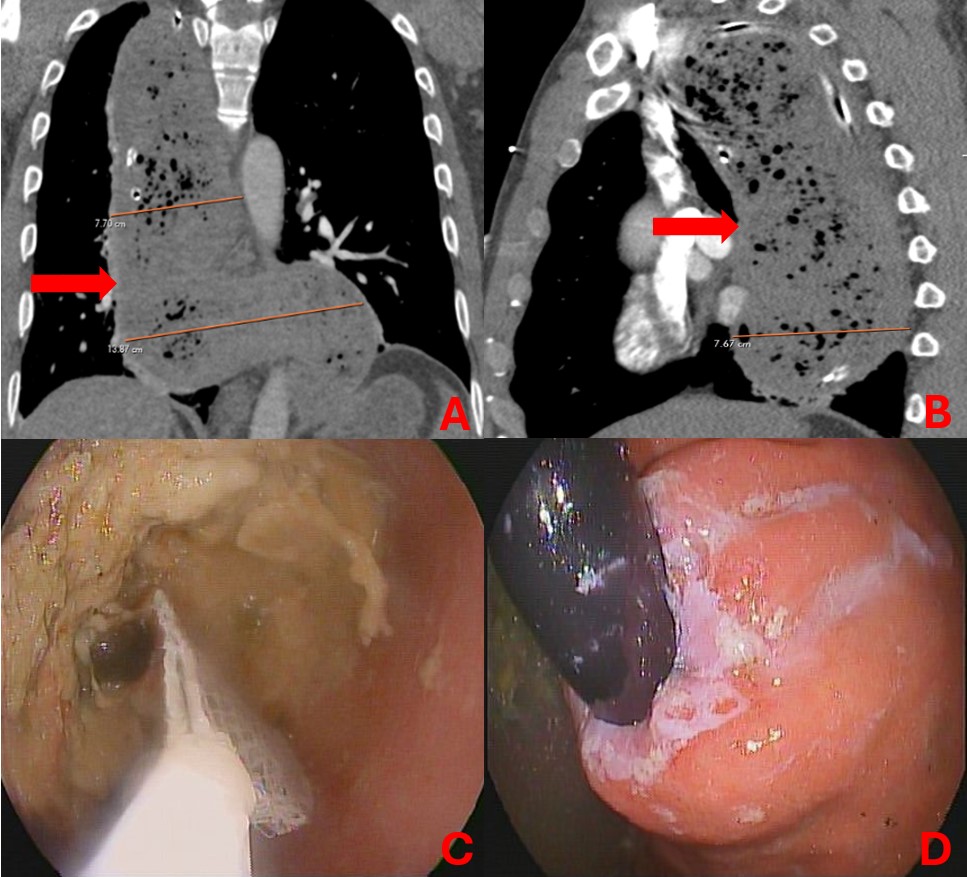
Case Description/Methods: A 52-year-old man with a history of multiple episodes of achalasia presented for shortness of breath. His family noted he had an episode of food impaction the night before. Despite continuous positive airway pressure and inhaler treatments, the patient was hypoxic to 82% with severe respiratory distress and was subsequently intubated. CT of the chest showed a severely dilated, food-filled, and tortuous esophagus.
EGD confirmed the CT findings along with an esophageal ulcer and a hypertrophied LES. The debris was removed over the course of 2 procedural days with Roth nets and suction. LES dilation was met with mild resistance but was ultimately successful. The patient was extubated the next day and discharged on a clear liquid diet with planned outpatient follow-up to pursue potential myotomy.
Discussion: The etiology of achalasia is not completely understood but believed to be related to the damage of the myenteric plexus which can stem from autoimmune factors, viral infections, or other unknown causes. It is common to see respiratory symptoms with 40% of patients complaining of wheezing and dyspnea. However, respiratory failure itself is a much rarer issue, with only around 50 cases documented since 1950. Unlike our patient, previously described cases had no prior history of achalasia. Our patient presented with a severely dilated esophagus resulting in compressive atelectasis and an esophageal ulcer suggesting chronic mucosal irritation and ischemia.
It is hypothesized that the patient experienced severe symptoms due to the incomplete treatment of the initial incident. Although he received a dilation this admission, this patient and others should be warned that achalasia can reoccur. Since there are no current guidelines for surveillance EGDs for achalasia, these patients should be encouraged to visit a provider when symptoms start to reappear. However, in some refractory cases despite active monitoring, management requires LES botulinum injections or surgical myotomies. This patient’s severe achalasia and intubation could have been avoided with a thorough education on warning signs and providers being aware of this long-term management strategy.
Disclosures:
Rohan Patil, BS1, Jacob Pierce. Reitnauer, BS1, Kazi T. Haque, MD2, Patrick Boddie, MD3, Fernando Sosa, BS1, Sean Ngo, BS1, Rohan Ahuja, MD1, Iyad Al-bustami, MD, MPH(c)4, Ruth Bell, DO5, Kevin K. Yu, MD1, Andrew Dupont, MD, MSPH5. P0585 - Achalasia's Tight Chokehold on Breath and Life! A Case of Severe, Compressive Achalasia Causing Acute Respiratory Failure, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Health, McGovern Medical School, Houston, TX; 2University of Texas Health, McGovern Medical School, Pearland, TX; 3Baylor College of Medicine, Houston, TX; 4Brooklyn Hospital Center, Houston, TX; 5McGovern Medical School at UTHealth, Houston, TX
Introduction: Achalasia is characterized by progressive esophageal dysmotility resulting in the incomplete relaxation of the lower esophageal sphincter (LES) and dysfunctional peristalsis. We present a patient who developed respiratory failure requiring endotracheal intubation due to massive food impaction secondary to severe achalasia.
Case Description/Methods: A 52-year-old man with a history of multiple episodes of achalasia presented for shortness of breath. His family noted he had an episode of food impaction the night before. Despite continuous positive airway pressure and inhaler treatments, the patient was hypoxic to 82% with severe respiratory distress and was subsequently intubated. CT of the chest showed a severely dilated, food-filled, and tortuous esophagus.
EGD confirmed the CT findings along with an esophageal ulcer and a hypertrophied LES. The debris was removed over the course of 2 procedural days with Roth nets and suction. LES dilation was met with mild resistance but was ultimately successful. The patient was extubated the next day and discharged on a clear liquid diet with planned outpatient follow-up to pursue potential myotomy.
Discussion: The etiology of achalasia is not completely understood but believed to be related to the damage of the myenteric plexus which can stem from autoimmune factors, viral infections, or other unknown causes. It is common to see respiratory symptoms with 40% of patients complaining of wheezing and dyspnea. However, respiratory failure itself is a much rarer issue, with only around 50 cases documented since 1950. Unlike our patient, previously described cases had no prior history of achalasia. Our patient presented with a severely dilated esophagus resulting in compressive atelectasis and an esophageal ulcer suggesting chronic mucosal irritation and ischemia.
It is hypothesized that the patient experienced severe symptoms due to the incomplete treatment of the initial incident. Although he received a dilation this admission, this patient and others should be warned that achalasia can reoccur. Since there are no current guidelines for surveillance EGDs for achalasia, these patients should be encouraged to visit a provider when symptoms start to reappear. However, in some refractory cases despite active monitoring, management requires LES botulinum injections or surgical myotomies. This patient’s severe achalasia and intubation could have been avoided with a thorough education on warning signs and providers being aware of this long-term management strategy.
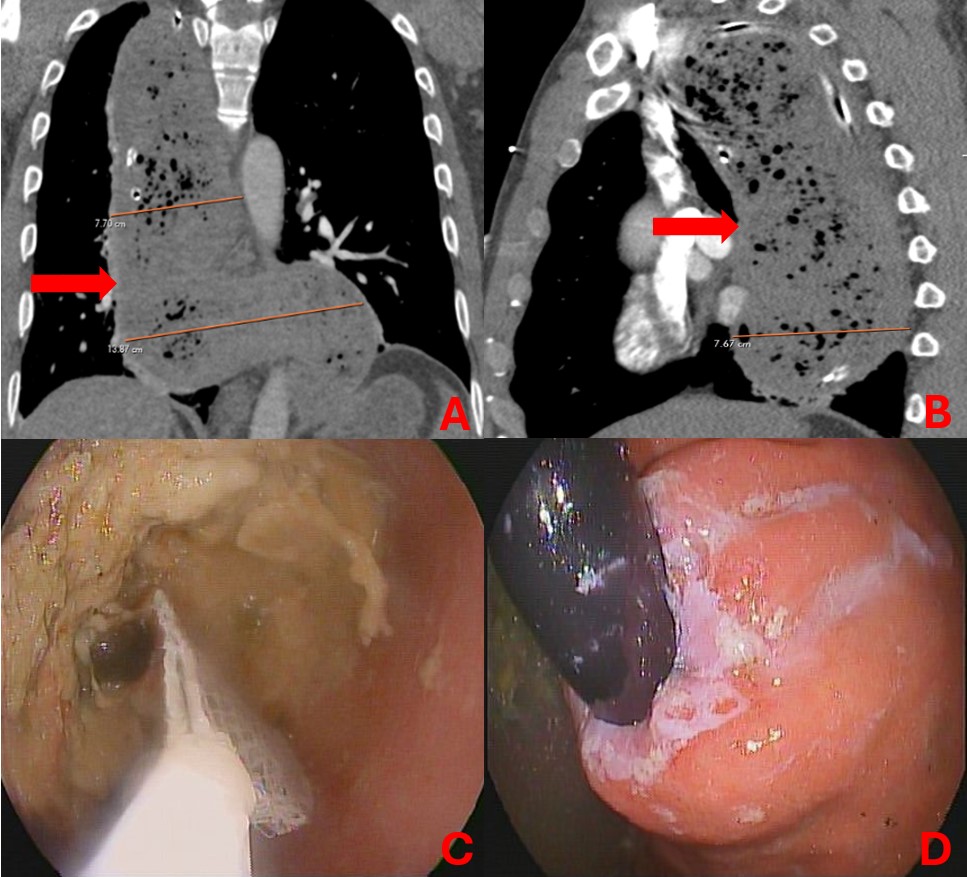
Figure: Figure 1:
a) A coronal slice of CT Chest showing a dilated, tortuous esophagus labeled by the red arrow. Maximal width was 7.70 cm at T4 spinal level and 13.87 cm at the T11 spinal level.
b) A sagittal slice of CT Chest showing the compressive nature of the severe achalasia, leading to respiratory failure. Maximal depth depicted 7.67 cm from anterior wall of the esophagus to the posterior wall.
c) Endoscopic image showing a Roth net attempting to remove food debris in the esophagus.
d) Endoscopic image showing a severely hypertrophied lower esophageal sphincter on endoscopic retroflexion.
a) A coronal slice of CT Chest showing a dilated, tortuous esophagus labeled by the red arrow. Maximal width was 7.70 cm at T4 spinal level and 13.87 cm at the T11 spinal level.
b) A sagittal slice of CT Chest showing the compressive nature of the severe achalasia, leading to respiratory failure. Maximal depth depicted 7.67 cm from anterior wall of the esophagus to the posterior wall.
c) Endoscopic image showing a Roth net attempting to remove food debris in the esophagus.
d) Endoscopic image showing a severely hypertrophied lower esophageal sphincter on endoscopic retroflexion.
Disclosures:
Rohan Patil indicated no relevant financial relationships.
Jacob Reitnauer indicated no relevant financial relationships.
Kazi Haque indicated no relevant financial relationships.
Patrick Boddie indicated no relevant financial relationships.
Fernando Sosa indicated no relevant financial relationships.
Sean Ngo indicated no relevant financial relationships.
Rohan Ahuja indicated no relevant financial relationships.
Iyad Al-bustami indicated no relevant financial relationships.
Ruth Bell indicated no relevant financial relationships.
Kevin Yu indicated no relevant financial relationships.
Andrew Dupont indicated no relevant financial relationships.
Rohan Patil, BS1, Jacob Pierce. Reitnauer, BS1, Kazi T. Haque, MD2, Patrick Boddie, MD3, Fernando Sosa, BS1, Sean Ngo, BS1, Rohan Ahuja, MD1, Iyad Al-bustami, MD, MPH(c)4, Ruth Bell, DO5, Kevin K. Yu, MD1, Andrew Dupont, MD, MSPH5. P0585 - Achalasia's Tight Chokehold on Breath and Life! A Case of Severe, Compressive Achalasia Causing Acute Respiratory Failure, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
