Sunday Poster Session
Category: Esophagus
P0588 - Taken With a Grain of Salt: How Untreated Achalasia Led to Severe Hypernatremia
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Ali Ismail, MD
Penn Medicine
Philadelphia, PA
Presenting Author(s)
Ali Ismail, MD1, Michael Demarco, DO1, Veena Madhu, MD1, Anila Vasireddy, MD2, Hiba Hameed, MD1
1Penn Medicine, Philadelphia, PA; 2University of Pennsylvania Health System, Philadelphia, PA
Introduction: Achalasia is a rare esophageal motility disorder characterized by the degeneration of the myenteric plexus, resulting in failure of relaxation of the lower esophageal sphincter and the absence of esophageal peristalsis. The etiology of primary achalasia is typically unknown, however secondary achalasia has been linked to certain autoimmune disorders, parasitic and viral infections, and infiltrative processes, among others.
Case Description/Methods: Here we present the case of a 35-year-old female who was admitted to our hospital with a 3 day history of progressive confusion and somnolence and was found to be severely hypernatremic with a sodium level of 179 necessitating ICU admission.
Her symptoms initially began 12 months earlier when she developed dysphagia, vomiting, and regurgitation which were attributed to her recent pregnancy. During the pregnancy, her symptoms remained mild and she delivered her child uneventfully. However, in the postpartum period her symptoms progressed rapidly leading to a 70 lb weight loss over 4 months. During this period she had multiple hospital admissions for vomiting, during one of these visits she underwent a barium study, EGD, and Esophageal Manometry which diagnosed her with type 1 achalasia. However, she left against medical advice before receiving any treatment and her care was further complicated by poor follow up. Her symptoms continued to worsen at home, eventually leading to this ICU admission.
In the ICU she received hypotonic fluids with D5 ¼ saline, resulting in the correction of her electrolyte abnormalities and subsequent improvement in her mental status. Multiple discussions were held with the patient regarding her treatment options, and she ultimately opted for Botox as a temporizing measure while she determined her longterm treatment plan.
Discussion: Achalasia is rare, with limited documented instances leading to such profound dehydration and hypernatremia. The patient's clinical course leads to multiple points of discussion; first, her symptoms started during the peripartum period and were initially attributed to pregnancy and GERD, however, her dysphagia and regurgitation were atypical for these conditions and this led to a delay in diagnosis. Secondly, her symptoms worsened postpartum. While the effect of pregnancy on achalasia has not been well studied, other cases have also reported this. This case highlights the importance of early recognition of achalasia in patients presenting with atypical GI symptoms during and after pregnancy.

Disclosures:
Ali Ismail, MD1, Michael Demarco, DO1, Veena Madhu, MD1, Anila Vasireddy, MD2, Hiba Hameed, MD1. P0588 - Taken With a Grain of Salt: How Untreated Achalasia Led to Severe Hypernatremia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Penn Medicine, Philadelphia, PA; 2University of Pennsylvania Health System, Philadelphia, PA
Introduction: Achalasia is a rare esophageal motility disorder characterized by the degeneration of the myenteric plexus, resulting in failure of relaxation of the lower esophageal sphincter and the absence of esophageal peristalsis. The etiology of primary achalasia is typically unknown, however secondary achalasia has been linked to certain autoimmune disorders, parasitic and viral infections, and infiltrative processes, among others.
Case Description/Methods: Here we present the case of a 35-year-old female who was admitted to our hospital with a 3 day history of progressive confusion and somnolence and was found to be severely hypernatremic with a sodium level of 179 necessitating ICU admission.
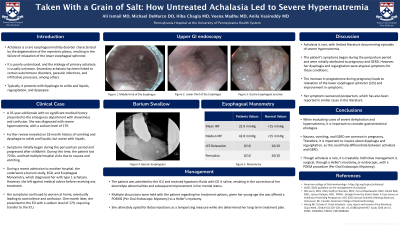
Her symptoms initially began 12 months earlier when she developed dysphagia, vomiting, and regurgitation which were attributed to her recent pregnancy. During the pregnancy, her symptoms remained mild and she delivered her child uneventfully. However, in the postpartum period her symptoms progressed rapidly leading to a 70 lb weight loss over 4 months. During this period she had multiple hospital admissions for vomiting, during one of these visits she underwent a barium study, EGD, and Esophageal Manometry which diagnosed her with type 1 achalasia. However, she left against medical advice before receiving any treatment and her care was further complicated by poor follow up. Her symptoms continued to worsen at home, eventually leading to this ICU admission.
In the ICU she received hypotonic fluids with D5 ¼ saline, resulting in the correction of her electrolyte abnormalities and subsequent improvement in her mental status. Multiple discussions were held with the patient regarding her treatment options, and she ultimately opted for Botox as a temporizing measure while she determined her longterm treatment plan.
Discussion: Achalasia is rare, with limited documented instances leading to such profound dehydration and hypernatremia. The patient's clinical course leads to multiple points of discussion; first, her symptoms started during the peripartum period and were initially attributed to pregnancy and GERD, however, her dysphagia and regurgitation were atypical for these conditions and this led to a delay in diagnosis. Secondly, her symptoms worsened postpartum. While the effect of pregnancy on achalasia has not been well studied, other cases have also reported this. This case highlights the importance of early recognition of achalasia in patients presenting with atypical GI symptoms during and after pregnancy.

Figure: Barium Esophagram
Disclosures:
Ali Ismail indicated no relevant financial relationships.
Michael Demarco indicated no relevant financial relationships.
Veena Madhu indicated no relevant financial relationships.
Anila Vasireddy indicated no relevant financial relationships.
Hiba Hameed indicated no relevant financial relationships.
Ali Ismail, MD1, Michael Demarco, DO1, Veena Madhu, MD1, Anila Vasireddy, MD2, Hiba Hameed, MD1. P0588 - Taken With a Grain of Salt: How Untreated Achalasia Led to Severe Hypernatremia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
