Sunday Poster Session
Category: Esophagus
P0517 - Diagnostic Accuracy and Grading of Esophagitis – A cross-sectional analytic study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- JJ
Jason John, MD
University of South Florida Morsani College of Medicine
Orlando, FL
Presenting Author(s)
Jason John, MD1, Pushpak Taunk, MD2, John Jacobs, MD, FACG3, Wojciech Blonski, MD, PhD4, Athanasios Tsalatsanis, PhD5, Ambuj Kumar, MD, MPH3
1University of South Florida Morsani College of Medicine, Orlando, FL; 2University of South Florida, Tampa, FL; 3University of South Florida Morsani College of Medicine, Tampa, FL; 4University of South Florida, James A. Haley VA Hospital, Tampa, FL; 5University of South Florida Health, Tampa, FL
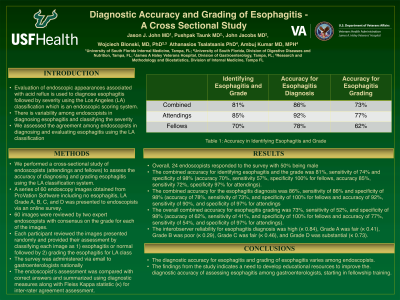
Introduction: Evaluation of endoscopic appearances associated with acid reflux is used to diagnose esophagitis followed by severity using the Los Angeles (LA) classification which is an endoscopic scoring system. There is variability among endoscopists in diagnosing esophagitis and classifying the severity. We assessed the agreement among endoscopists in diagnosing and evaluating esophagitis using the LA classification system.
Methods: We performed a cross-sectional study of endoscopists (attendings and fellows) to assess the accuracy of diagnosing and grading esophagitis using the LA classification system. A series of 60 endoscopy images obtained from ProVation Software including no esophagitis, LA Grade A, B, C, and D was presented to endoscopists via an online survey. Each participant reviewed the images presented randomly and provided their assessment by classifying each image as 1) esophagitis or normal followed by 2) grading the esophagitis for LA class. The survey was administered via email to gastroenterologists nationally. The endoscopist’s assessment was compared with correct answers and summarized using diagnostic measures along with Fleiss Kappa statistic (κ) for inter-rater agreement assessment.
Results: Overall, 24 endoscopists responded to the survey with 50% being male. The combined accuracy for identifying esophagitis and the grade was 81%, sensitivity of 74% and specificity of 98% (accuracy 70%, sensitivity 57%, specificity 100% for fellows accuracy 85%, sensitivity 72%, specificity 97% for attendings). The accuracy for the esophagitis diagnosis was 86%, sensitivity of 86% and specificity of 98% (accuracy of 78%, sensitivity of 73%, and specificity of 100% for fellows and accuracy of 92%, sensitivity of 90%, and specificity of 97% for attendings. The overall accuracy for esophagitis grading was 73%, sensitivity of 52%, and specificity of 98% (accuracy of 62%, sensitivity of 41%, and specificity of 100% for fellows and accuracy of 77%, sensitivity of 54%, and specificity of 97% for attendings). The interobserver reliability for esophagitis diagnosis was high (κ 0.84), Grade A was fair (κ 0.41), Grade B was poor (κ 0.29), Grade C was fair (κ 0.46), and Grade D was substantial (κ 0.73).
Discussion: The diagnostic accuracy for esophagitis and grading of esophagitis varies among endoscopists. The findings from the study indicates a need to develop educational resources to improve the diagnostic accuracy of assessing esophagitis among gastroenterologists, starting in fellowship training.
Disclosures:
Jason John, MD1, Pushpak Taunk, MD2, John Jacobs, MD, FACG3, Wojciech Blonski, MD, PhD4, Athanasios Tsalatsanis, PhD5, Ambuj Kumar, MD, MPH3. P0517 - Diagnostic Accuracy and Grading of Esophagitis – A cross-sectional analytic study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of South Florida Morsani College of Medicine, Orlando, FL; 2University of South Florida, Tampa, FL; 3University of South Florida Morsani College of Medicine, Tampa, FL; 4University of South Florida, James A. Haley VA Hospital, Tampa, FL; 5University of South Florida Health, Tampa, FL
Introduction: Evaluation of endoscopic appearances associated with acid reflux is used to diagnose esophagitis followed by severity using the Los Angeles (LA) classification which is an endoscopic scoring system. There is variability among endoscopists in diagnosing esophagitis and classifying the severity. We assessed the agreement among endoscopists in diagnosing and evaluating esophagitis using the LA classification system.
Methods: We performed a cross-sectional study of endoscopists (attendings and fellows) to assess the accuracy of diagnosing and grading esophagitis using the LA classification system. A series of 60 endoscopy images obtained from ProVation Software including no esophagitis, LA Grade A, B, C, and D was presented to endoscopists via an online survey. Each participant reviewed the images presented randomly and provided their assessment by classifying each image as 1) esophagitis or normal followed by 2) grading the esophagitis for LA class. The survey was administered via email to gastroenterologists nationally. The endoscopist’s assessment was compared with correct answers and summarized using diagnostic measures along with Fleiss Kappa statistic (κ) for inter-rater agreement assessment.
Results: Overall, 24 endoscopists responded to the survey with 50% being male. The combined accuracy for identifying esophagitis and the grade was 81%, sensitivity of 74% and specificity of 98% (accuracy 70%, sensitivity 57%, specificity 100% for fellows accuracy 85%, sensitivity 72%, specificity 97% for attendings). The accuracy for the esophagitis diagnosis was 86%, sensitivity of 86% and specificity of 98% (accuracy of 78%, sensitivity of 73%, and specificity of 100% for fellows and accuracy of 92%, sensitivity of 90%, and specificity of 97% for attendings. The overall accuracy for esophagitis grading was 73%, sensitivity of 52%, and specificity of 98% (accuracy of 62%, sensitivity of 41%, and specificity of 100% for fellows and accuracy of 77%, sensitivity of 54%, and specificity of 97% for attendings). The interobserver reliability for esophagitis diagnosis was high (κ 0.84), Grade A was fair (κ 0.41), Grade B was poor (κ 0.29), Grade C was fair (κ 0.46), and Grade D was substantial (κ 0.73).
Discussion: The diagnostic accuracy for esophagitis and grading of esophagitis varies among endoscopists. The findings from the study indicates a need to develop educational resources to improve the diagnostic accuracy of assessing esophagitis among gastroenterologists, starting in fellowship training.
Disclosures:
Jason John indicated no relevant financial relationships.
Pushpak Taunk: Boston Scientific – Consultant. Neptune Medical – Consultant.
John Jacobs: Medtronic – Consultant. Regeneron – Speakers Bureau. Sanofi/Genzyme – Speakers Bureau.
Wojciech Blonski indicated no relevant financial relationships.
Athanasios Tsalatsanis indicated no relevant financial relationships.
Ambuj Kumar indicated no relevant financial relationships.
Jason John, MD1, Pushpak Taunk, MD2, John Jacobs, MD, FACG3, Wojciech Blonski, MD, PhD4, Athanasios Tsalatsanis, PhD5, Ambuj Kumar, MD, MPH3. P0517 - Diagnostic Accuracy and Grading of Esophagitis – A cross-sectional analytic study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

