Sunday Poster Session
Category: Esophagus
P0521 - Understanding the Natural History of Patients With Barrett's Esophagus and Eosinophilic Esophagitis: A Case Series
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Aaron Yazdian, MD
Vanderbilt University Medical Center
Nashville, TN
Presenting Author(s)
Aaron Yazdian, MD, Muhammad Hayat, MD, Krutika Patel, MBBS, Yash Choksi, MD
Vanderbilt University Medical Center, Nashville, TN
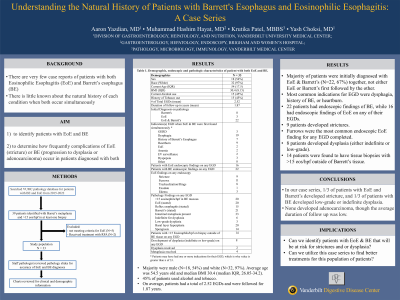
Introduction: There are very few case reports of patients with both Eosinophilic Esophagitis (EoE) and Barrett’s esophagus (BE), and there is little known about the natural history of each condition when both occur simultaneously. We aim: 1) to identify patients with EoE and BE, and 2) to determine how frequently complications of EoE (stricture) or BE (progression to dysplasia or adenocarcinoma) occur in patients diagnosed with both.
Methods: At our medical center, we searched the pathology database for patients with BE and EoE from 2015-2022 using natural language processing terms “Barrett’s and eosinophilic esophagitis.” We manually reviewed the results from this search and identified 39 patients who had Barrett’s metaplasia and >15 eosinophils/high power field in at least one biopsy. Patients treated with RFA were not included since RFA can induce esophageal eosinophilia; thus, 33 patients were included in the study. A staff pathologist reviewed the pathology slides for accuracy of EoE and BE diagnoses. Patients were chart reviewed for demographics, number of EGDs and EGD findings, pathology, treatment, treatment response, symptoms and development of cancer.
Results: Our study population was majority male (N=18, 54%) and white (N=32, 97%). Average age was 54.5 years old and median BMI 30.4 (median IQR, 26.05-34.2). 45% of patients used alcohol and tobacco. On average, patients had a total of 2.52 EGDs and were followed for 1.87 years. The majority of patients were initially diagnosed with EoE & Barrett’s (N=22, 67%) together, not either EoE or Barrett’s first followed by the other. The most common indications for EGD were dysphagia, history of BE, or heartburn. 22 patients had endoscopic findings of BE, while 16 had endoscopic findings of EoE on any of their EGDs. 9 patients developed strictures. Furrows were the most common EoE finding on EGD. 8 patients developed dysplasia (either indefinite or low-grade). 14 patients were found to have tissue biopsies with >15 eos/hpf outside of barrett’s tissue.
Discussion: In our case series, 1/3 of patients with EoE and Barrett’s developed stricture, and 1/3 of patients with BE developed low-grade or indefinite dysplasia. None developed adenocarcinoma, though the average duration of follow up was low.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Aaron Yazdian, MD, Muhammad Hayat, MD, Krutika Patel, MBBS, Yash Choksi, MD. P0521 - Understanding the Natural History of Patients With Barrett's Esophagus and Eosinophilic Esophagitis: A Case Series, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Vanderbilt University Medical Center, Nashville, TN
Introduction: There are very few case reports of patients with both Eosinophilic Esophagitis (EoE) and Barrett’s esophagus (BE), and there is little known about the natural history of each condition when both occur simultaneously. We aim: 1) to identify patients with EoE and BE, and 2) to determine how frequently complications of EoE (stricture) or BE (progression to dysplasia or adenocarcinoma) occur in patients diagnosed with both.
Methods: At our medical center, we searched the pathology database for patients with BE and EoE from 2015-2022 using natural language processing terms “Barrett’s and eosinophilic esophagitis.” We manually reviewed the results from this search and identified 39 patients who had Barrett’s metaplasia and >15 eosinophils/high power field in at least one biopsy. Patients treated with RFA were not included since RFA can induce esophageal eosinophilia; thus, 33 patients were included in the study. A staff pathologist reviewed the pathology slides for accuracy of EoE and BE diagnoses. Patients were chart reviewed for demographics, number of EGDs and EGD findings, pathology, treatment, treatment response, symptoms and development of cancer.
Results: Our study population was majority male (N=18, 54%) and white (N=32, 97%). Average age was 54.5 years old and median BMI 30.4 (median IQR, 26.05-34.2). 45% of patients used alcohol and tobacco. On average, patients had a total of 2.52 EGDs and were followed for 1.87 years. The majority of patients were initially diagnosed with EoE & Barrett’s (N=22, 67%) together, not either EoE or Barrett’s first followed by the other. The most common indications for EGD were dysphagia, history of BE, or heartburn. 22 patients had endoscopic findings of BE, while 16 had endoscopic findings of EoE on any of their EGDs. 9 patients developed strictures. Furrows were the most common EoE finding on EGD. 8 patients developed dysplasia (either indefinite or low-grade). 14 patients were found to have tissue biopsies with >15 eos/hpf outside of barrett’s tissue.
Discussion: In our case series, 1/3 of patients with EoE and Barrett’s developed stricture, and 1/3 of patients with BE developed low-grade or indefinite dysplasia. None developed adenocarcinoma, though the average duration of follow up was low.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Aaron Yazdian indicated no relevant financial relationships.
Muhammad Hayat indicated no relevant financial relationships.
Krutika Patel indicated no relevant financial relationships.
Yash Choksi indicated no relevant financial relationships.
Aaron Yazdian, MD, Muhammad Hayat, MD, Krutika Patel, MBBS, Yash Choksi, MD. P0521 - Understanding the Natural History of Patients With Barrett's Esophagus and Eosinophilic Esophagitis: A Case Series, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

