Sunday Poster Session
Category: Esophagus
P0527 - Tracheoesophageal Fistula and Esophageal Hyperpigmentation: Are These Incidental Findings During Upper Endoscopy?
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

James Barnett, MD
University of Texas at Houston
Houston, TX
Presenting Author(s)
James Barnett, MD1, Asmeen Bhatt, MD2, Eric D. Yoon, MD1
1University of Texas at Houston, Houston, TX; 2Center for Interventional Gastroenterology at UTHealth (iGUT), Houston, TX
Introduction: Tracheoesophageal fistula (TEF) is a rare endoscopic finding. We present a patient with melena and altered mental status (AMS), found to have esophageal hyperpigmentation and TEF on endoscopy.
Case Description/Methods: An 81-year-old female with past medical history of gastroesophageal reflux disease (GERD), atrial fibrillation, diabetes mellitus, and breast cancer was found by paramedics covered in melanic stool with 1 week of nausea, vomiting, diarrhea, decreased oral intake. On admission, vitals were significant for hypotension, labs were significant for a white blood cell count of 31.0K/uL, and lactic acid of 8.0mMol/L, physical exam was notable for AMS.
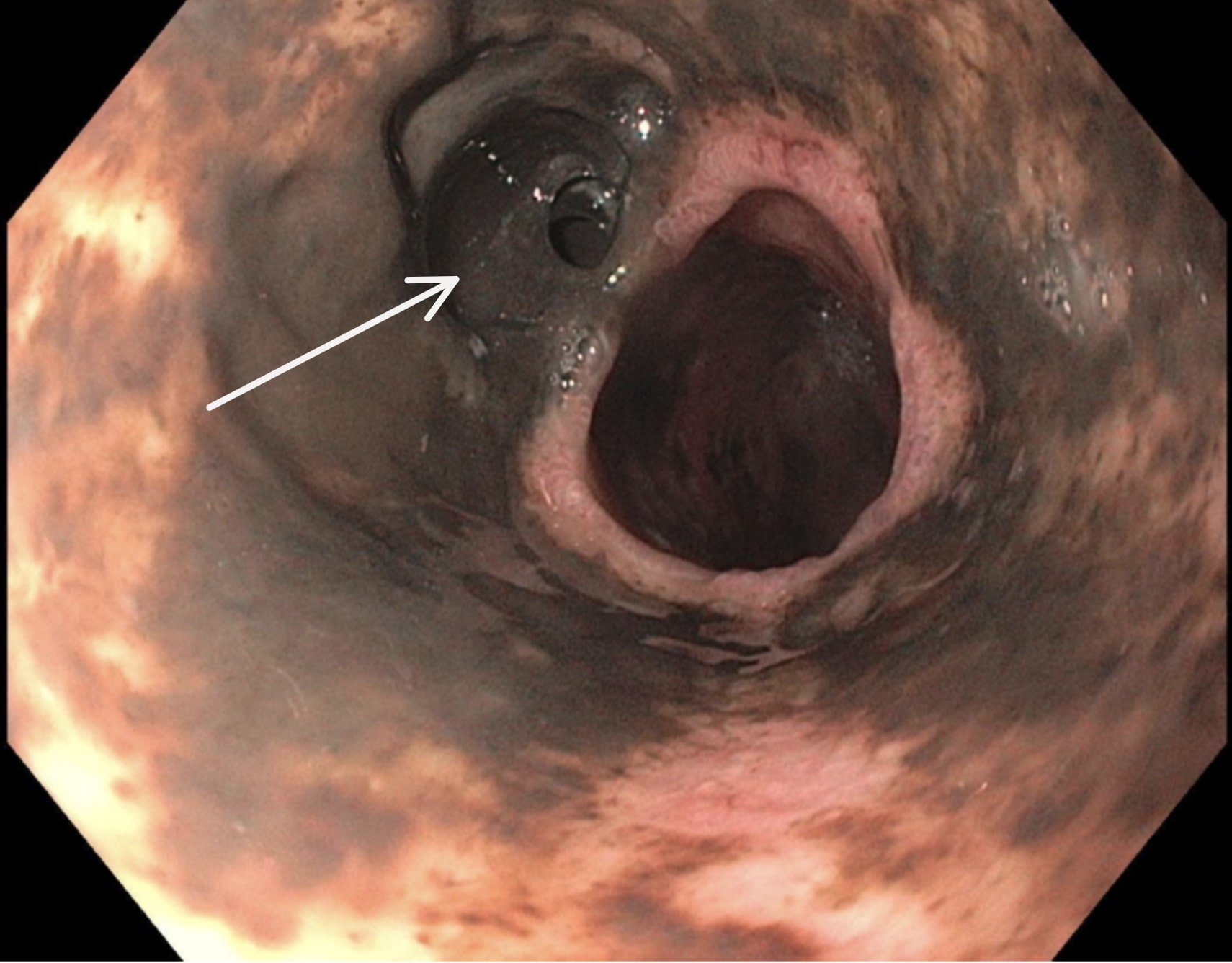
Upper endoscopy was performed revealing black macular lesions in the hypopharynx and esophagus. In the mid-proximal esophagus, a large circumferential ulceration with adjoining esophageal fistula without active bleeding was visualized (Figure1) and biopsied. The stomach and duodenum appeared normal. Pathology revealed severe acute and chronic inflammation, ulceration, and refractile brown crystalline material at the tissue surface. Computed tomography of the neck showed a lucency between the distal trachea and esophagus, consistent with TEF. Bronchoscopy failed to reveal the TEF, which can happen if the fistula connects to a smaller bronchus.
Discussion: Acquired TEF is a rare endoscopic finding and literature on this topic is primarily from case reports. Although this patient's history was limited, she likely had several risk factors which led to TEF. She may have had chemotherapy and radiation exposure as a part of breast cancer treatment, which are independent risk factors for secondary TEF. Other risk factors for TEF revolve around local inflammation or ischemia caused by prolonged endotracheal intubation, chronic GERD, embolus from atrial fibrillation. Clinically significant bleeding is not associated with TEF. Hemoptysis is a known symptom of TEF, however her melena was likely from another source not seen on endoscopy. The esophageal hyperpigmentation seen in this case is a rare finding in and of itself. Hyperpigmentation is not associated with TEF, but both can result from chronic inflammation. Biopsy ruled out other causes of color change such as melanosis. Ferrous sulfate ingestion is a known culprit of local crystalline deposition and inflammation, but her home medications were unknown. The endoscopic findings for this patient are rare, in the setting of insufficient patient history, the possible etiologies are vast.
Disclosures:
James Barnett, MD1, Asmeen Bhatt, MD2, Eric D. Yoon, MD1. P0527 - Tracheoesophageal Fistula and Esophageal Hyperpigmentation: Are These Incidental Findings During Upper Endoscopy?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas at Houston, Houston, TX; 2Center for Interventional Gastroenterology at UTHealth (iGUT), Houston, TX
Introduction: Tracheoesophageal fistula (TEF) is a rare endoscopic finding. We present a patient with melena and altered mental status (AMS), found to have esophageal hyperpigmentation and TEF on endoscopy.
Case Description/Methods: An 81-year-old female with past medical history of gastroesophageal reflux disease (GERD), atrial fibrillation, diabetes mellitus, and breast cancer was found by paramedics covered in melanic stool with 1 week of nausea, vomiting, diarrhea, decreased oral intake. On admission, vitals were significant for hypotension, labs were significant for a white blood cell count of 31.0K/uL, and lactic acid of 8.0mMol/L, physical exam was notable for AMS.
Upper endoscopy was performed revealing black macular lesions in the hypopharynx and esophagus. In the mid-proximal esophagus, a large circumferential ulceration with adjoining esophageal fistula without active bleeding was visualized (Figure1) and biopsied. The stomach and duodenum appeared normal. Pathology revealed severe acute and chronic inflammation, ulceration, and refractile brown crystalline material at the tissue surface. Computed tomography of the neck showed a lucency between the distal trachea and esophagus, consistent with TEF. Bronchoscopy failed to reveal the TEF, which can happen if the fistula connects to a smaller bronchus.
Discussion: Acquired TEF is a rare endoscopic finding and literature on this topic is primarily from case reports. Although this patient's history was limited, she likely had several risk factors which led to TEF. She may have had chemotherapy and radiation exposure as a part of breast cancer treatment, which are independent risk factors for secondary TEF. Other risk factors for TEF revolve around local inflammation or ischemia caused by prolonged endotracheal intubation, chronic GERD, embolus from atrial fibrillation. Clinically significant bleeding is not associated with TEF. Hemoptysis is a known symptom of TEF, however her melena was likely from another source not seen on endoscopy. The esophageal hyperpigmentation seen in this case is a rare finding in and of itself. Hyperpigmentation is not associated with TEF, but both can result from chronic inflammation. Biopsy ruled out other causes of color change such as melanosis. Ferrous sulfate ingestion is a known culprit of local crystalline deposition and inflammation, but her home medications were unknown. The endoscopic findings for this patient are rare, in the setting of insufficient patient history, the possible etiologies are vast.
Figure: Endoscopic image of the mid-proximal esophagus showing hyperpigmentation and esophageal fistula (White Arrow).
Disclosures:
James Barnett indicated no relevant financial relationships.
Asmeen Bhatt indicated no relevant financial relationships.
Eric Yoon indicated no relevant financial relationships.
James Barnett, MD1, Asmeen Bhatt, MD2, Eric D. Yoon, MD1. P0527 - Tracheoesophageal Fistula and Esophageal Hyperpigmentation: Are These Incidental Findings During Upper Endoscopy?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
