Sunday Poster Session
Category: Esophagus
P0529 - An Unexpected Gastrointestinal Complication of Atrial Fibrillation Ablation Leading to a Fatal Outcome
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Rohan Ahuja, MD
University of Texas Health, McGovern Medical School
Houston, TX
Presenting Author(s)
Rohan Ahuja, MD1, Vijay Aaroha Kandula, MD, PharmD2, Jacob Pierce. Reitnauer, BS1, Rohan Patil, BS1, Kazi T. Haque, MD3, Mindy Chen, MD2, Faisal Ali, MD1, Tanima Jana, MD, FACG1
1University of Texas Health, McGovern Medical School, Houston, TX; 2University of Texas at Houston, Houston, TX; 3University of Texas Health, McGovern Medical School, Pearland, TX
Introduction: Atrial fibrillation (AF) radiofrequency ablation (RFA) procedures are increasingly used as treatments for persistent AF. Esophageal perforation and atrio-esophageal fistulization (AEF) are rare but serious complications of RFA that carry a high mortality rate. We present a case of a 53-year-old man who developed an AEF after a RFA procedure complicated by GI bleeding, and ultimately death from cardiac compromise.
Case Description/Methods: A 53-year-old patient with a history of non-ischemic cardiomyopathy, persistent AF, hypertension, and diabetes mellitus presented after syncope secondary to AF. Urgent AF ablation was pursued. Despite a return to sinus rhythm, complications after RFA included PEA cardiac arrest, pneumonia, embolic stroke, seizures, and coffee-ground output from his nasogastric tube.
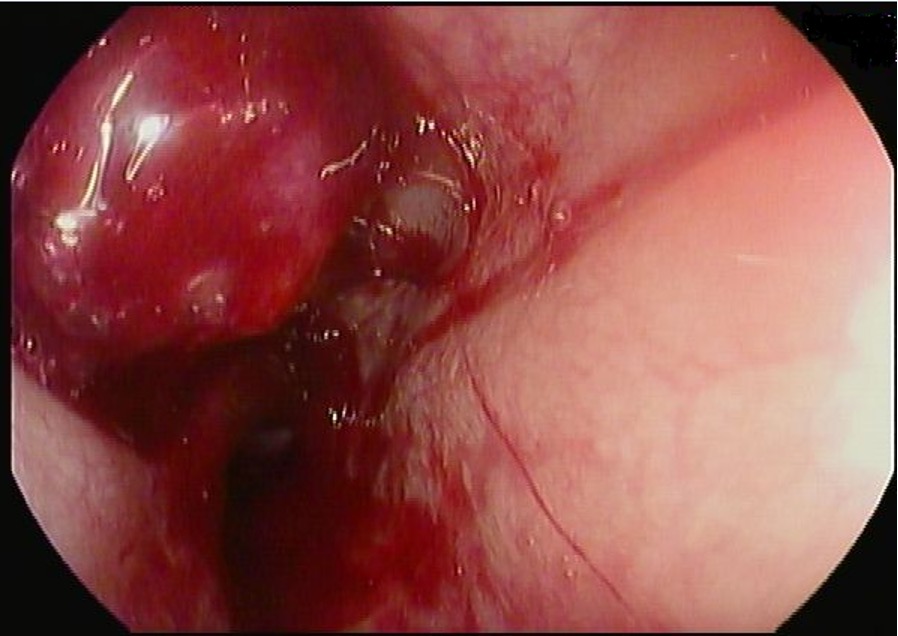
Due to the coffee-ground output, gastroenterology (GI) was consulted. Initial upper endoscopy (EGD) revealed a large, deep mid-esophageal ulcer treated conservatively with IV proton pump inhibitor therapy. The GI service was later reconsulted for evaluation of worsening anemia and melena. Repeat EGD showed a large, pulsatile mass with active oozing protruding into the lumen of the esophagus (Figure 1). Due to the clinical instability of the patient, the procedure was terminated. Emergent CT angiography of the chest showed an esophageal ulcer bulging into the posterior aspect of the left atrium, with concerns for a contained perforation and fistulous connection between the ulcer and the left atrium. Cardiothoracic surgery evaluated the patient and determined that he was not a surgical candidate due to his poor clinical status and multiple medical comorbidities. Due to his declining status, he was transitioned to comfort care. Pertinent autopsy results included esophageal ulceration and a right ventricle transmural defect.
Discussion: This case demonstrates a rare adverse event from RFA of AF that carries a high mortality rate. The proximity of the esophagus to the posterior wall of the left atrium places the esophagus at risk for thermal injury during an ablation procedure. The Kansas City classification of esophageal injury after AF ablation can be helpful with predicting clinical outcomes. At the time of the final endoscopy, our patient’s esophageal injury had already progressed to type 3b injury (perforation with AEF). Our patient’s clinical presentation highlights the importance of being aware of the potential gastrointestinal complications that can arise from AF ablation procedures.
Disclosures:
Rohan Ahuja, MD1, Vijay Aaroha Kandula, MD, PharmD2, Jacob Pierce. Reitnauer, BS1, Rohan Patil, BS1, Kazi T. Haque, MD3, Mindy Chen, MD2, Faisal Ali, MD1, Tanima Jana, MD, FACG1. P0529 - An Unexpected Gastrointestinal Complication of Atrial Fibrillation Ablation Leading to a Fatal Outcome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Health, McGovern Medical School, Houston, TX; 2University of Texas at Houston, Houston, TX; 3University of Texas Health, McGovern Medical School, Pearland, TX
Introduction: Atrial fibrillation (AF) radiofrequency ablation (RFA) procedures are increasingly used as treatments for persistent AF. Esophageal perforation and atrio-esophageal fistulization (AEF) are rare but serious complications of RFA that carry a high mortality rate. We present a case of a 53-year-old man who developed an AEF after a RFA procedure complicated by GI bleeding, and ultimately death from cardiac compromise.
Case Description/Methods: A 53-year-old patient with a history of non-ischemic cardiomyopathy, persistent AF, hypertension, and diabetes mellitus presented after syncope secondary to AF. Urgent AF ablation was pursued. Despite a return to sinus rhythm, complications after RFA included PEA cardiac arrest, pneumonia, embolic stroke, seizures, and coffee-ground output from his nasogastric tube.
Due to the coffee-ground output, gastroenterology (GI) was consulted. Initial upper endoscopy (EGD) revealed a large, deep mid-esophageal ulcer treated conservatively with IV proton pump inhibitor therapy. The GI service was later reconsulted for evaluation of worsening anemia and melena. Repeat EGD showed a large, pulsatile mass with active oozing protruding into the lumen of the esophagus (Figure 1). Due to the clinical instability of the patient, the procedure was terminated. Emergent CT angiography of the chest showed an esophageal ulcer bulging into the posterior aspect of the left atrium, with concerns for a contained perforation and fistulous connection between the ulcer and the left atrium. Cardiothoracic surgery evaluated the patient and determined that he was not a surgical candidate due to his poor clinical status and multiple medical comorbidities. Due to his declining status, he was transitioned to comfort care. Pertinent autopsy results included esophageal ulceration and a right ventricle transmural defect.
Discussion: This case demonstrates a rare adverse event from RFA of AF that carries a high mortality rate. The proximity of the esophagus to the posterior wall of the left atrium places the esophagus at risk for thermal injury during an ablation procedure. The Kansas City classification of esophageal injury after AF ablation can be helpful with predicting clinical outcomes. At the time of the final endoscopy, our patient’s esophageal injury had already progressed to type 3b injury (perforation with AEF). Our patient’s clinical presentation highlights the importance of being aware of the potential gastrointestinal complications that can arise from AF ablation procedures.
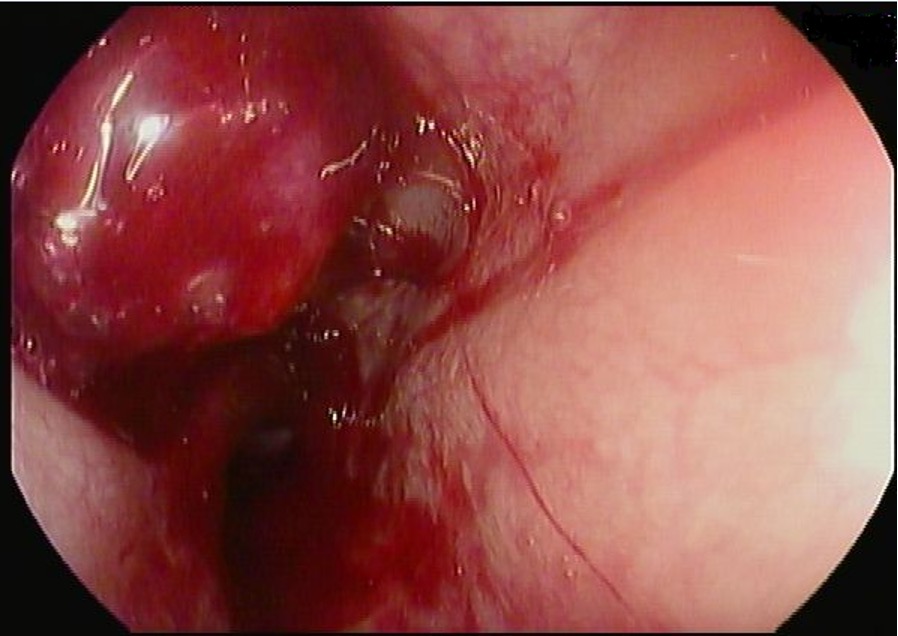
Figure: Atrio-esophageal Fistula in mid-esophagus
Disclosures:
Rohan Ahuja indicated no relevant financial relationships.
Vijay Aaroha Kandula indicated no relevant financial relationships.
Jacob Reitnauer indicated no relevant financial relationships.
Rohan Patil indicated no relevant financial relationships.
Kazi Haque indicated no relevant financial relationships.
Mindy Chen indicated no relevant financial relationships.
Faisal Ali indicated no relevant financial relationships.
Tanima Jana indicated no relevant financial relationships.
Rohan Ahuja, MD1, Vijay Aaroha Kandula, MD, PharmD2, Jacob Pierce. Reitnauer, BS1, Rohan Patil, BS1, Kazi T. Haque, MD3, Mindy Chen, MD2, Faisal Ali, MD1, Tanima Jana, MD, FACG1. P0529 - An Unexpected Gastrointestinal Complication of Atrial Fibrillation Ablation Leading to a Fatal Outcome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
