Sunday Poster Session
Category: Colon
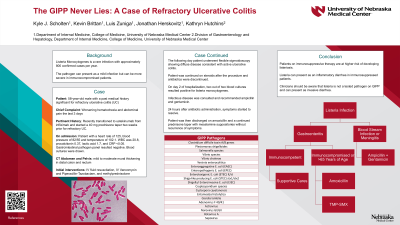
P0356 - The GIPP Never Lies: A Case of Refractory Ulcerative Colitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Kyle Scholten, DO
University of Nebraska Medical Center
Omaha, NE
Presenting Author(s)
Award: Presidential Poster Award
Kyle Scholten, DO, Luis Zuniga, DO, Kevin Brittan, MD, Jonathan Herskovitz, MD, PhD, Kathryn Hutchins, MD
University of Nebraska Medical Center, Omaha, NE
Introduction: Listeria monocytogenes is a rare infection with approximately 1500 confirmed cases per year. It is an opportunistic facultative intracellular parasite that primarily infects via ingestion of contaminated food with subsequent intestinal mucosal involvement. The pathogen traditionally presents as a mild infection but can be more severe in immunocompromised patients. A Gastrointestinal pathogen panel (GIPP) is a valuable diagnostic tool, especially in inflammatory hemorrhagic diarrhea; however, its utility is limited to tested pathogens. We present a case of invasive listeriosis in an ulcerative colitis patient.
Case Description/Methods: A 58-year-old male with a past medical history significant for refractory ulcerative colitis (UC) presented to the emergency department after 3-days of worsening hematochezia and abdominal pain. The patient had transitioned to Ustekinumab from Infliximab and started a 40 mg prednisone taper two weeks prior due to refractory UC symptoms. On admission, heart rate was 125, blood pressure was 82/55, and temperature was 102.1°F. Pertinent labs included white blood cell count 20.8, procalcitonin 0.37, lactic acid 1.7, and CRP < 0.5. The patient was given fluids and broad-spectrum antibiotics along with methylprednisolone. CT was significant for mild to moderate mural thickening in the distal colon and rectum. Gastrointestinal pathogen panel (GIPP) was negative. Flexible sigmoidoscopy the following day revealed diffuse disease consistent with an active ulcerative colitis flare. On hospital day two, 2/2 blood cultures were positive for Listeria monocytogenes. Infectious disease was consulted, and the patient was treated with ampicillin and gentamicin. Following treatment initiation, hematochezia decreased, and abdominal pain subsided. The patient was discharged on amoxicillin with a continued prednisone taper and mesalamine suppositories without recurrence of symptoms.
Discussion: Clinicians should be aware that Listeria monocytogenes, a potentially fatal opportunistic foodborne infection, is not routinely tested on a GI pathogen panel and may manifest primarily as invasive diarrhea. Patients on immunosuppressive therapies are at greater risk of developing serious manifestations of listeriosis, such as sepsis, meningitis, or death. Listeria monocytogenes should be on a clinician’s differential diagnosis of foodborne gastrointestinal pathogens causing refractory inflammatory diarrhea.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kyle Scholten, DO, Luis Zuniga, DO, Kevin Brittan, MD, Jonathan Herskovitz, MD, PhD, Kathryn Hutchins, MD. P0356 - The GIPP Never Lies: A Case of Refractory Ulcerative Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Kyle Scholten, DO, Luis Zuniga, DO, Kevin Brittan, MD, Jonathan Herskovitz, MD, PhD, Kathryn Hutchins, MD
University of Nebraska Medical Center, Omaha, NE
Introduction: Listeria monocytogenes is a rare infection with approximately 1500 confirmed cases per year. It is an opportunistic facultative intracellular parasite that primarily infects via ingestion of contaminated food with subsequent intestinal mucosal involvement. The pathogen traditionally presents as a mild infection but can be more severe in immunocompromised patients. A Gastrointestinal pathogen panel (GIPP) is a valuable diagnostic tool, especially in inflammatory hemorrhagic diarrhea; however, its utility is limited to tested pathogens. We present a case of invasive listeriosis in an ulcerative colitis patient.
Case Description/Methods: A 58-year-old male with a past medical history significant for refractory ulcerative colitis (UC) presented to the emergency department after 3-days of worsening hematochezia and abdominal pain. The patient had transitioned to Ustekinumab from Infliximab and started a 40 mg prednisone taper two weeks prior due to refractory UC symptoms. On admission, heart rate was 125, blood pressure was 82/55, and temperature was 102.1°F. Pertinent labs included white blood cell count 20.8, procalcitonin 0.37, lactic acid 1.7, and CRP < 0.5. The patient was given fluids and broad-spectrum antibiotics along with methylprednisolone. CT was significant for mild to moderate mural thickening in the distal colon and rectum. Gastrointestinal pathogen panel (GIPP) was negative. Flexible sigmoidoscopy the following day revealed diffuse disease consistent with an active ulcerative colitis flare. On hospital day two, 2/2 blood cultures were positive for Listeria monocytogenes. Infectious disease was consulted, and the patient was treated with ampicillin and gentamicin. Following treatment initiation, hematochezia decreased, and abdominal pain subsided. The patient was discharged on amoxicillin with a continued prednisone taper and mesalamine suppositories without recurrence of symptoms.
Discussion: Clinicians should be aware that Listeria monocytogenes, a potentially fatal opportunistic foodborne infection, is not routinely tested on a GI pathogen panel and may manifest primarily as invasive diarrhea. Patients on immunosuppressive therapies are at greater risk of developing serious manifestations of listeriosis, such as sepsis, meningitis, or death. Listeria monocytogenes should be on a clinician’s differential diagnosis of foodborne gastrointestinal pathogens causing refractory inflammatory diarrhea.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kyle Scholten indicated no relevant financial relationships.
Luis Zuniga indicated no relevant financial relationships.
Kevin Brittan indicated no relevant financial relationships.
Jonathan Herskovitz indicated no relevant financial relationships.
Kathryn Hutchins indicated no relevant financial relationships.
Kyle Scholten, DO, Luis Zuniga, DO, Kevin Brittan, MD, Jonathan Herskovitz, MD, PhD, Kathryn Hutchins, MD. P0356 - The GIPP Never Lies: A Case of Refractory Ulcerative Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

