Sunday Poster Session
Category: Colon
P0362 - The Unseen Challenge: Confronting Anorectal Melanoma
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Alison N. Lawrence, BA
University of California Irvine School of Medicine
Irvine, CA
Presenting Author(s)
Alison N. Lawrence, BA1, Rishi Vermani, BS2, Erica Duh, MD3, C Gregory Albers, MD2, Valery Vilchez Parra, MD4, Christina Ling, MD2
1University of California Irvine School of Medicine, Irvine, CA; 2University of California, Irvine, Orange, CA; 3University of California Irvine Digestive Health Institute, Orange, CA; 4UCI, Orange, CA
Introduction: Anorectal mucosal melanoma (AMM) is rare, making up 0.05 percent of colorectal malignancies and 1 percent of anal canal cancers. Although AMM pathogenesis is unknown, human immunodeficiency virus infection may be a risk factor. This report describes a case of rapidly progressing AMM resulting in near-complete bowel obstruction.
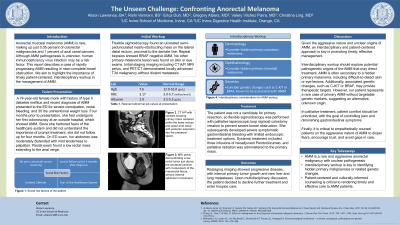
Case Description/Methods: A 74-year-old female monk with history of type II diabetes mellitus and recent diagnosis of AMM presented to the ED for severe constipation, rectal bleeding, and 30 lbs unintentional weight loss. Four months prior to presentation, she underwent her first colonoscopy at an outside hospital, which showed AMM. Since she did not understand the importance of prompt treatment, she did not follow up for four months. On exam, her abdomen was moderately distended with mild tenderness to palpation. Rectal exam found low rectal mass extending to the anal verge. Flexible sigmoidoscopy found an ulcerated semi-pedunculated nearly-obstructing mass on the lateral distal rectum, proximal to the dentate line. Repeat biopsies showed BRAF negative AMM. No other primary melanoma lesion was found. Initial staging imaging including CT A/P, MRI pelvis (Fig. 1), and PET/CT demonstrated locally advanced T3a-b malignancy without distant metastasis. The patient was not a candidate for primary resection, so palliative laparoscopic loop sigmoid colostomy was performed. She subsequently developed severe symptomatic gastrointestinal bleeding with limited endoscopic treatment options. She received three infusions of neoadjuvant Pembrolizumab and palliative radiation to the primary mass. Two months later, restaging imaging showed progressive disease with liver and lung metastases. Upon multidisciplinary discussion, she decided to decline further treatment and enter hospice.
Discussion: Given the aggressive nature and unclear origins of AMM, an interdisciplinary and patient-centered approach is key in promoting timely, effective management. Workup should focus on exploring potential pathogenetic origins, including hidden primary skin and eye lesions or genetic changes, such as C-KIT or BRAF, that could provide potential treatment targets. In palliative treatment, patient comfort should be prioritized, with the goal of controlling pain and diminishing gastrointestinal symptoms. Furthermore, it is critical to empathetically counsel patients on the aggressive nature of AMM to dispel fears and encourage trust, potentially avoiding large gaps in care.

Disclosures:
Alison N. Lawrence, BA1, Rishi Vermani, BS2, Erica Duh, MD3, C Gregory Albers, MD2, Valery Vilchez Parra, MD4, Christina Ling, MD2. P0362 - The Unseen Challenge: Confronting Anorectal Melanoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of California Irvine School of Medicine, Irvine, CA; 2University of California, Irvine, Orange, CA; 3University of California Irvine Digestive Health Institute, Orange, CA; 4UCI, Orange, CA
Introduction: Anorectal mucosal melanoma (AMM) is rare, making up 0.05 percent of colorectal malignancies and 1 percent of anal canal cancers. Although AMM pathogenesis is unknown, human immunodeficiency virus infection may be a risk factor. This report describes a case of rapidly progressing AMM resulting in near-complete bowel obstruction.
Case Description/Methods: A 74-year-old female monk with history of type II diabetes mellitus and recent diagnosis of AMM presented to the ED for severe constipation, rectal bleeding, and 30 lbs unintentional weight loss. Four months prior to presentation, she underwent her first colonoscopy at an outside hospital, which showed AMM. Since she did not understand the importance of prompt treatment, she did not follow up for four months. On exam, her abdomen was moderately distended with mild tenderness to palpation. Rectal exam found low rectal mass extending to the anal verge. Flexible sigmoidoscopy found an ulcerated semi-pedunculated nearly-obstructing mass on the lateral distal rectum, proximal to the dentate line. Repeat biopsies showed BRAF negative AMM. No other primary melanoma lesion was found. Initial staging imaging including CT A/P, MRI pelvis (Fig. 1), and PET/CT demonstrated locally advanced T3a-b malignancy without distant metastasis. The patient was not a candidate for primary resection, so palliative laparoscopic loop sigmoid colostomy was performed. She subsequently developed severe symptomatic gastrointestinal bleeding with limited endoscopic treatment options. She received three infusions of neoadjuvant Pembrolizumab and palliative radiation to the primary mass. Two months later, restaging imaging showed progressive disease with liver and lung metastases. Upon multidisciplinary discussion, she decided to decline further treatment and enter hospice.
Discussion: Given the aggressive nature and unclear origins of AMM, an interdisciplinary and patient-centered approach is key in promoting timely, effective management. Workup should focus on exploring potential pathogenetic origins, including hidden primary skin and eye lesions or genetic changes, such as C-KIT or BRAF, that could provide potential treatment targets. In palliative treatment, patient comfort should be prioritized, with the goal of controlling pain and diminishing gastrointestinal symptoms. Furthermore, it is critical to empathetically counsel patients on the aggressive nature of AMM to dispel fears and encourage trust, potentially avoiding large gaps in care.

Figure: Fig. 1: MRI pelvis demonstrating a low rectal tumor just above the anorectal junction with involvement of the mesorectal fascia and suspicious superior rectal lymphadenopathy.
Disclosures:
Alison Lawrence indicated no relevant financial relationships.
Rishi Vermani indicated no relevant financial relationships.
Erica Duh indicated no relevant financial relationships.
C Gregory Albers: Nestle Health – Speakers Bureau. Phathom Pharmaceuticals – Speakers Bureau. Salix Pharmaceuticals – Speakers Bureau.
Valery Vilchez Parra indicated no relevant financial relationships.
Christina Ling indicated no relevant financial relationships.
Alison N. Lawrence, BA1, Rishi Vermani, BS2, Erica Duh, MD3, C Gregory Albers, MD2, Valery Vilchez Parra, MD4, Christina Ling, MD2. P0362 - The Unseen Challenge: Confronting Anorectal Melanoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
