Sunday Poster Session
Category: Colon
P0258 - CAR T-Cell Therapy-Induced Pseudomembranous Colitis Mimicking C. difficile Infection
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Rukaiya Bashir hamidu, MD
University of Maryland Medical Center
Baltimore, MD
Presenting Author(s)
Rukaiya Bashir hamidu, MD1, Erik Von Rosenvinge, MD2
1University of Maryland Medical Center, Baltimore, MD; 2University of Maryland School of Medicine, Baltimore, MD
Introduction: Chimeric antigen receptor T-cell therapy (CAR T) and immune checkpoint inhibitors (ICIs) are increasingly used in cancer treatment. While ICI-induced colitis is well recognized, CAR T-associated colitis is rare. Pseudomembranous colitis is commonly associated with Clostridioides difficile infection (CDI) but can have other causes. We report a case of diarrhea with pseudomembranous colitis after CAR T successfully treated with budesonide.
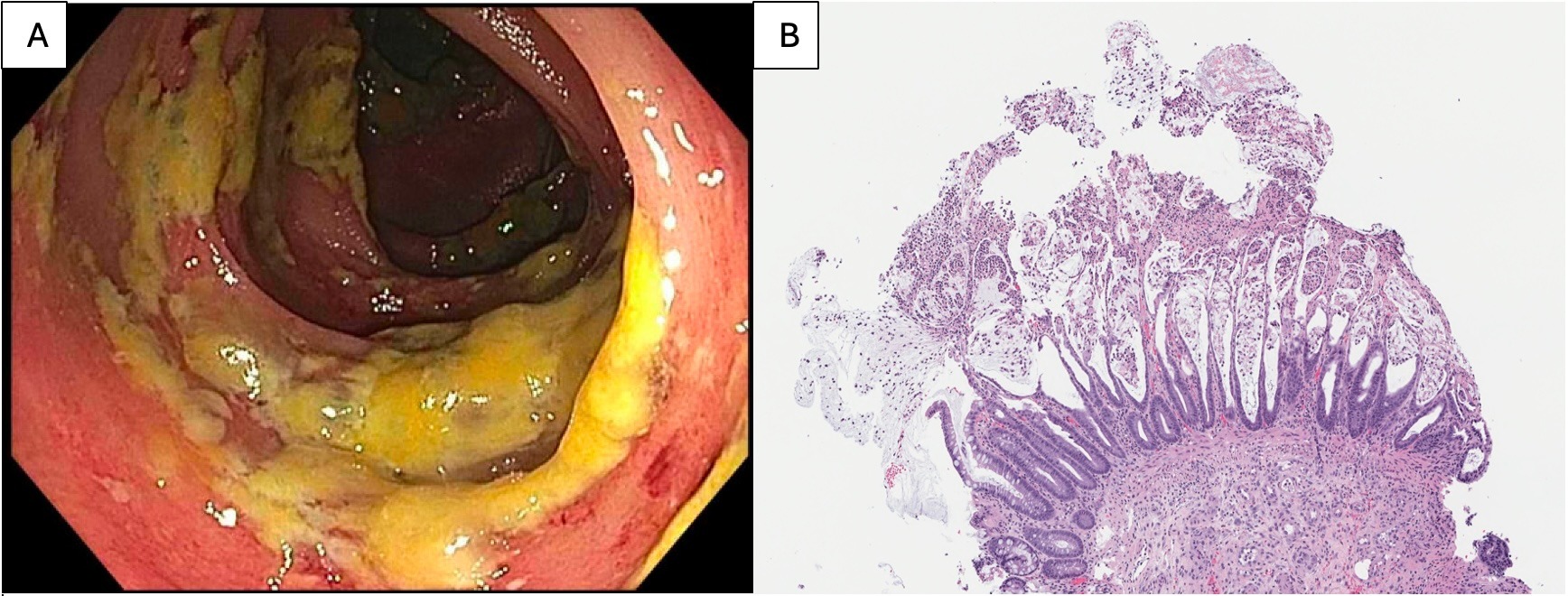
Case Description/Methods: A 67-year-old female was hospitalized for acute diarrhea 9 weeks after ciltacabtagene autoleucel CAR T infusion for relapsed multiple myeloma. Post-infusion she developed cytokine release syndrome and Bell’s palsy, treated with steroids but resulting in severe steroid-myopathy. Initial evaluation revealed mild colitis on CT scan with positive stool PCR for C. difficile gene but negative toxins A and B on enzyme immunoassay. Fidaxomicin for presumed CDI failed to resolve diarrhea prompting colonoscopy on day 10, which revealed pseudomembranous exudates in the transverse colon (Figure A), confirmed via biopsies (Figure B). This led to retreatment with oral vancomycin despite negative repeat stool tests for CDI. Diarrhea however persisted, necessitating supplemental parenteral nutrition. Further examination of her medical history and literature uncovered rare instances of colitis after CAR T, with one case responding to prednisone and vedolizumab. Limiting systemic steroids due to recent steroid myopathy, oral budesonide (controlled-ileal release) was started, and her diarrhea rapidly resolved. Four months post-discharge, budesonide was tapered off without recurrence of diarrhea.
Discussion: Only two prior cases of colitis after CAR T have been reported, both presenting with diarrhea like this case but differing in endoscopic findings and implicated CAR T agents (tisagenlecleucel and axicabtagene ciloleucel). Likewise, pseudomembranous colitis is rarely associated with non-CDI causes like medications. This marks the 3rd reported case of CAR T-associated colitis, the 1st linked to ciltacabtagene autoleucel, and highlights the importance of considering CAR T in the differential diagnosis for diarrhea. Budesonide should also be considered for treatment in similar cases. Furthermore, in cases of pseudomembranous colitis (PC) with ambiguous CDI testing and poor response to antibiotics, considering rare causes of PC is crucial for timely diagnosis, facilitating appropriate treatment, and preventing unnecessary escalation of anti-CDI antibiotics.
Disclosures:
Rukaiya Bashir hamidu, MD1, Erik Von Rosenvinge, MD2. P0258 - CAR T-Cell Therapy-Induced Pseudomembranous Colitis Mimicking <i>C. difficile</i> Infection, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Maryland Medical Center, Baltimore, MD; 2University of Maryland School of Medicine, Baltimore, MD
Introduction: Chimeric antigen receptor T-cell therapy (CAR T) and immune checkpoint inhibitors (ICIs) are increasingly used in cancer treatment. While ICI-induced colitis is well recognized, CAR T-associated colitis is rare. Pseudomembranous colitis is commonly associated with Clostridioides difficile infection (CDI) but can have other causes. We report a case of diarrhea with pseudomembranous colitis after CAR T successfully treated with budesonide.
Case Description/Methods: A 67-year-old female was hospitalized for acute diarrhea 9 weeks after ciltacabtagene autoleucel CAR T infusion for relapsed multiple myeloma. Post-infusion she developed cytokine release syndrome and Bell’s palsy, treated with steroids but resulting in severe steroid-myopathy. Initial evaluation revealed mild colitis on CT scan with positive stool PCR for C. difficile gene but negative toxins A and B on enzyme immunoassay. Fidaxomicin for presumed CDI failed to resolve diarrhea prompting colonoscopy on day 10, which revealed pseudomembranous exudates in the transverse colon (Figure A), confirmed via biopsies (Figure B). This led to retreatment with oral vancomycin despite negative repeat stool tests for CDI. Diarrhea however persisted, necessitating supplemental parenteral nutrition. Further examination of her medical history and literature uncovered rare instances of colitis after CAR T, with one case responding to prednisone and vedolizumab. Limiting systemic steroids due to recent steroid myopathy, oral budesonide (controlled-ileal release) was started, and her diarrhea rapidly resolved. Four months post-discharge, budesonide was tapered off without recurrence of diarrhea.
Discussion: Only two prior cases of colitis after CAR T have been reported, both presenting with diarrhea like this case but differing in endoscopic findings and implicated CAR T agents (tisagenlecleucel and axicabtagene ciloleucel). Likewise, pseudomembranous colitis is rarely associated with non-CDI causes like medications. This marks the 3rd reported case of CAR T-associated colitis, the 1st linked to ciltacabtagene autoleucel, and highlights the importance of considering CAR T in the differential diagnosis for diarrhea. Budesonide should also be considered for treatment in similar cases. Furthermore, in cases of pseudomembranous colitis (PC) with ambiguous CDI testing and poor response to antibiotics, considering rare causes of PC is crucial for timely diagnosis, facilitating appropriate treatment, and preventing unnecessary escalation of anti-CDI antibiotics.
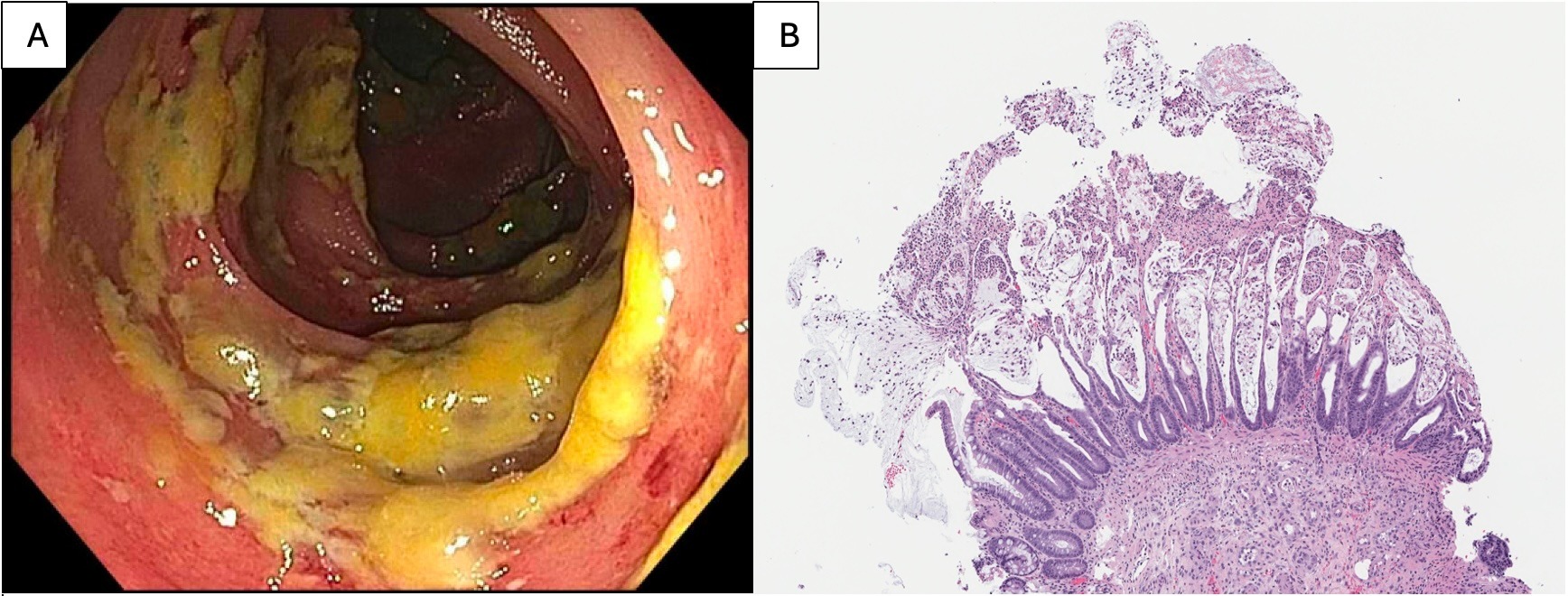
Figure: Figure A: Colonoscopy findings showing erythematous and pseudomembrane-covered mucosa in the transverse colon. Figure B: Histopathological examination of transverse colon mucosal biopsy (photomicrograph at 20x magnification, H&E stain) showing colonic mucosa with a focal area of ballooned crypts lacking.
Disclosures:
Rukaiya Bashir hamidu indicated no relevant financial relationships.
Erik Von Rosenvinge indicated no relevant financial relationships.
Rukaiya Bashir hamidu, MD1, Erik Von Rosenvinge, MD2. P0258 - CAR T-Cell Therapy-Induced Pseudomembranous Colitis Mimicking <i>C. difficile</i> Infection, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
