Sunday Poster Session
Category: Colon
P0261 - Salmonella Colitis Masquerading as Ulcerative Colitis Flare
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Brandon T. Wiggins, DO, MPH
Ascension Genesys Hospital
Grand Blanc, MI
Presenting Author(s)
Brandon T. Wiggins, DO, MPH1, Blace Haviland, DO2, Lina Ataya, MD3, Sonika K. Gill-Ahluwalia, DO4, Justin Miller, DO5
1Ascension Genesys Hospital, Grand Blanc, MI; 2Kettering Health, Dayton, OH; 3Ascension Genesys, Flushing, MI; 4Ascension Genesys, Rochester Hills, MI; 5Ascension Genesys Hospital, Clarkston, MI
Introduction: Ulcerative colitis (UC) is a chronic inflammatory bowel disease characterized by relapsing and remitting episodes of mucosal inflammation. Salmonella colitis in patients with longstanding ulcerative colitis poses a rare yet clinically significant challenge. The clinical features of UC flare and Salmonella colitis often overlap, complicating the differential diagnosis. In cases of persistent severe diarrhea despite appropriate treatment for UC, clinicians should consider the possibility of a concurrent infection.
Case Description/Methods: A 75 year old female with history of UC presented with diarrhea. The patient reported watery diarrhea every hour over the prior week without bleeding, pain or fevers.
She was diagnosed with UC 15 years prior and was controlled well on azathioprine and balsalazide without missed doses. Her last colonoscopy was 2 years prior to admission and demonstrated quiescent colitis.
Labs were remarkable for leukocytosis and elevated CRP. Urinalysis was positive for infection and she was started on antibiotics pending urine culture. Blood cultures, C. difficile, stool culture, and stool parasites were unremarkable.
Flexible sigmoidoscopy demonstrated multiple clean-based rectosigmoid ulcers that were not consistent with UC. Biopsies revealed active colitis with inflammatory changes and negative for dysplasia or viral inclusions. CT abdomen demonstrated acute descending colon colitis. Urine culture eventually returned positive for salmonella, raising suspicion for salmonella colitis and a stool PCR was pursued and positive. Ceftriaxone was switched to ciprofloxacin with resolution of symptoms and discharge.
Discussion: Salmonella is a gram-negative, facultative anaerobic Enterobacteriaceae known to cause diarrhea worldwide, as well as the leading cause of foodborne illness. Common foodborne exposures include poultry, eggs, and milk products.
Symptoms include bloody diarrhea, nausea and vomiting, fever, and possible abdominal cramping.
In a patient presenting with acute diarrhea, as seen in our case, non-typhoidal salmonella colitis is on the differential of infectious sources.The work-up of infectious colitis includes stool culture, blood culture, and/or stool PCR.
Management is often supportive due to the self limited nature in most cases. Supportive care is aimed at the replacement of fluids and electrolytes. Antibiotic therapy use is reserved for severe disease or those at risk of invasive disease, such as patients with UC.

Disclosures:
Brandon T. Wiggins, DO, MPH1, Blace Haviland, DO2, Lina Ataya, MD3, Sonika K. Gill-Ahluwalia, DO4, Justin Miller, DO5. P0261 - Salmonella Colitis Masquerading as Ulcerative Colitis Flare, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Ascension Genesys Hospital, Grand Blanc, MI; 2Kettering Health, Dayton, OH; 3Ascension Genesys, Flushing, MI; 4Ascension Genesys, Rochester Hills, MI; 5Ascension Genesys Hospital, Clarkston, MI
Introduction: Ulcerative colitis (UC) is a chronic inflammatory bowel disease characterized by relapsing and remitting episodes of mucosal inflammation. Salmonella colitis in patients with longstanding ulcerative colitis poses a rare yet clinically significant challenge. The clinical features of UC flare and Salmonella colitis often overlap, complicating the differential diagnosis. In cases of persistent severe diarrhea despite appropriate treatment for UC, clinicians should consider the possibility of a concurrent infection.
Case Description/Methods: A 75 year old female with history of UC presented with diarrhea. The patient reported watery diarrhea every hour over the prior week without bleeding, pain or fevers.
She was diagnosed with UC 15 years prior and was controlled well on azathioprine and balsalazide without missed doses. Her last colonoscopy was 2 years prior to admission and demonstrated quiescent colitis.
Labs were remarkable for leukocytosis and elevated CRP. Urinalysis was positive for infection and she was started on antibiotics pending urine culture. Blood cultures, C. difficile, stool culture, and stool parasites were unremarkable.
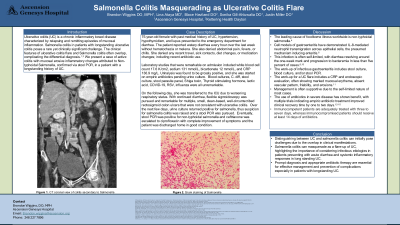
Flexible sigmoidoscopy demonstrated multiple clean-based rectosigmoid ulcers that were not consistent with UC. Biopsies revealed active colitis with inflammatory changes and negative for dysplasia or viral inclusions. CT abdomen demonstrated acute descending colon colitis. Urine culture eventually returned positive for salmonella, raising suspicion for salmonella colitis and a stool PCR was pursued and positive. Ceftriaxone was switched to ciprofloxacin with resolution of symptoms and discharge.
Discussion: Salmonella is a gram-negative, facultative anaerobic Enterobacteriaceae known to cause diarrhea worldwide, as well as the leading cause of foodborne illness. Common foodborne exposures include poultry, eggs, and milk products.
Symptoms include bloody diarrhea, nausea and vomiting, fever, and possible abdominal cramping.
In a patient presenting with acute diarrhea, as seen in our case, non-typhoidal salmonella colitis is on the differential of infectious sources.The work-up of infectious colitis includes stool culture, blood culture, and/or stool PCR.
Management is often supportive due to the self limited nature in most cases. Supportive care is aimed at the replacement of fluids and electrolytes. Antibiotic therapy use is reserved for severe disease or those at risk of invasive disease, such as patients with UC.

Figure: Coronal View Computed Tomography of Acute Long Segment Descending Colon Colitis
Disclosures:
Brandon Wiggins indicated no relevant financial relationships.
Blace Haviland indicated no relevant financial relationships.
Lina Ataya indicated no relevant financial relationships.
Sonika Gill-Ahluwalia indicated no relevant financial relationships.
Justin Miller indicated no relevant financial relationships.
Brandon T. Wiggins, DO, MPH1, Blace Haviland, DO2, Lina Ataya, MD3, Sonika K. Gill-Ahluwalia, DO4, Justin Miller, DO5. P0261 - Salmonella Colitis Masquerading as Ulcerative Colitis Flare, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
