Sunday Poster Session
Category: Colon
P0263 - Vanishing Act: Colonic Polyps Mimicking Tubular Adenoma Disappear With Resolution of Hypoxia
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Erica Loon, DO
University of Minnesota Medical Center
Minneapolis, MN
Presenting Author(s)
Erica Loon, DO1, Mohammad Bilal, MD2
1University of Minnesota Medical Center, Minneapolis, MN; 2University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Colonic mucosal prolapse are rare, benign polypoid lesions that arise from congestion, prolapse, or inflammation of the colon. These lesions can mimic dysplastic lesions endoscopically, leading to misdiagnosis and unnecessary interventions. Here, we present a patient with polypoid colonic lesions which were presumed to be adenomatous, that resolved with treatment of patient’s hypoxia.
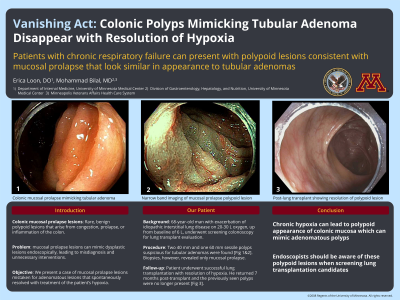
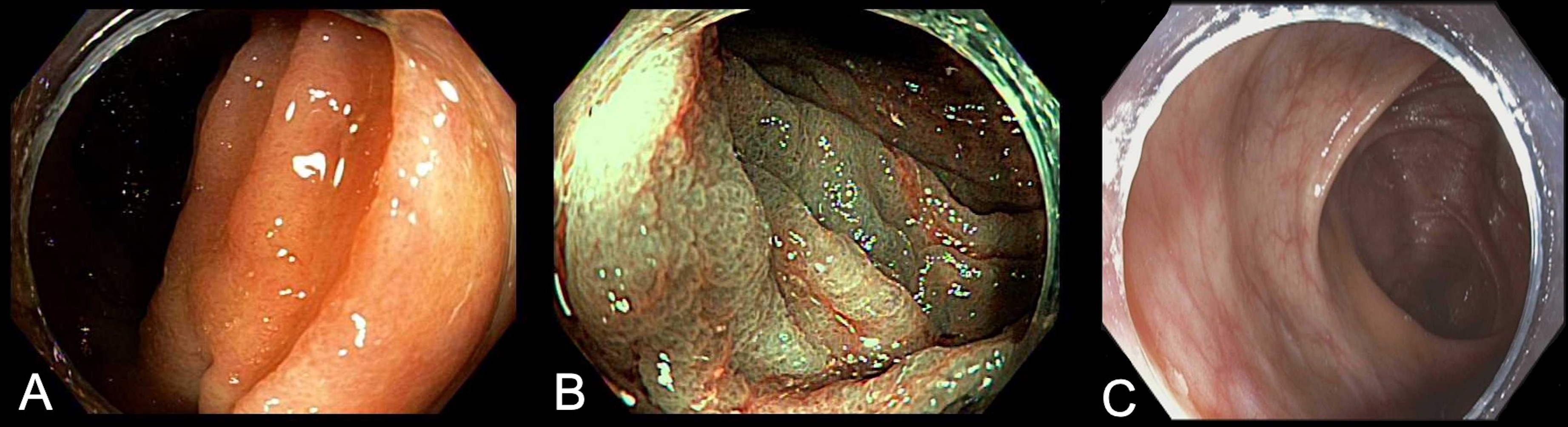
Case Description/Methods: A 68-year-old male with history of idiopathic interstitial lung disease (ILD), asthma, obstructive sleep apnea, and chronic eosinophilia with recurrent pneumonia, underwent screening colonoscopy as part of lung transplant evaluation after admission for ILD exacerbation. The patient had worsening respiratory status requiring 20-30 liters of high flow oxygen, which was an increase from his baseline requirement of six liters of oxygen. Colonoscopy was performed and multiple large polyps were seen as follows: 40 mm sessile polyp in the cecum, 60 mm sessile polyp in the ascending colon involving 50% of the colon circumference, and a 40 mm sessile polyp in the transverse colon. Narrow band imaging revealed features consistent with a tubular adenoma [Figure 1A&B]. It was deemed that these polypoid lesions were endoscopically resectable, however, given the patient's pulmonary condition, this was deferred. Biopsies were obtained to rule out submucosal invasive cancer prior to lung transplant. Pathology revealed mucosal prolapse without evidence of adenomatous glands or malignancy. Given the endoscopic appearance of these lesions, repeat colonoscopy with endoscopic mucosal resection was recommended post-lung transplant.
The patient underwent successful lung transplantation with resolution of hypoxia. Repeat colonoscopy was performed seven months post-transplant, and the previously seen polyps were no longer visualized [Figure 1C].
Discussion: Our case suggests that chronic hypoxia can lead to polypoid appearance of colonic mucosa which can be challenging to distinguish from adenomatous polyps. The polypoid colonic lesions completely resolved post-lung transplant, suggesting that these lesions developed due to inflammation from the patient’s acute on chronic hypoxia, and resolved with improved oxygen status post-transplant. These findings may have significant implications for patients undergoing colonoscopy as part of lung transplant evaluation, and, therefore, it is important for endoscopists to be aware of these rare findings in this patient population.
Disclosures:
Erica Loon, DO1, Mohammad Bilal, MD2. P0263 - Vanishing Act: Colonic Polyps Mimicking Tubular Adenoma Disappear With Resolution of Hypoxia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Minnesota Medical Center, Minneapolis, MN; 2University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Colonic mucosal prolapse are rare, benign polypoid lesions that arise from congestion, prolapse, or inflammation of the colon. These lesions can mimic dysplastic lesions endoscopically, leading to misdiagnosis and unnecessary interventions. Here, we present a patient with polypoid colonic lesions which were presumed to be adenomatous, that resolved with treatment of patient’s hypoxia.
Case Description/Methods: A 68-year-old male with history of idiopathic interstitial lung disease (ILD), asthma, obstructive sleep apnea, and chronic eosinophilia with recurrent pneumonia, underwent screening colonoscopy as part of lung transplant evaluation after admission for ILD exacerbation. The patient had worsening respiratory status requiring 20-30 liters of high flow oxygen, which was an increase from his baseline requirement of six liters of oxygen. Colonoscopy was performed and multiple large polyps were seen as follows: 40 mm sessile polyp in the cecum, 60 mm sessile polyp in the ascending colon involving 50% of the colon circumference, and a 40 mm sessile polyp in the transverse colon. Narrow band imaging revealed features consistent with a tubular adenoma [Figure 1A&B]. It was deemed that these polypoid lesions were endoscopically resectable, however, given the patient's pulmonary condition, this was deferred. Biopsies were obtained to rule out submucosal invasive cancer prior to lung transplant. Pathology revealed mucosal prolapse without evidence of adenomatous glands or malignancy. Given the endoscopic appearance of these lesions, repeat colonoscopy with endoscopic mucosal resection was recommended post-lung transplant.
The patient underwent successful lung transplantation with resolution of hypoxia. Repeat colonoscopy was performed seven months post-transplant, and the previously seen polyps were no longer visualized [Figure 1C].
Discussion: Our case suggests that chronic hypoxia can lead to polypoid appearance of colonic mucosa which can be challenging to distinguish from adenomatous polyps. The polypoid colonic lesions completely resolved post-lung transplant, suggesting that these lesions developed due to inflammation from the patient’s acute on chronic hypoxia, and resolved with improved oxygen status post-transplant. These findings may have significant implications for patients undergoing colonoscopy as part of lung transplant evaluation, and, therefore, it is important for endoscopists to be aware of these rare findings in this patient population.
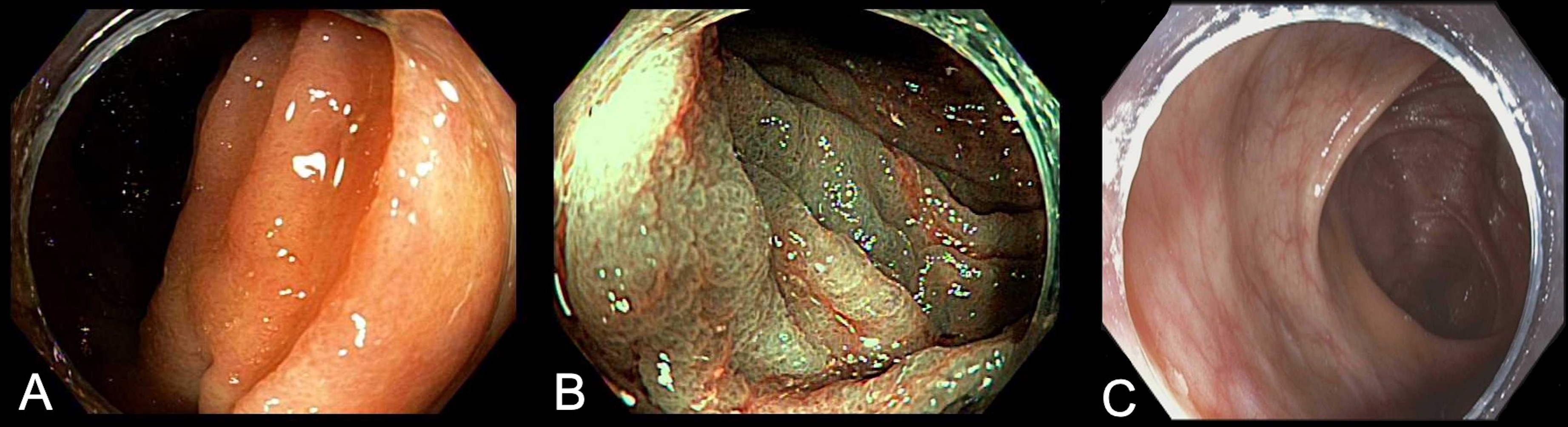
Figure: Figure 1. Colonic mucosal prolapse polyp mimicking tubular adenoma on endoscopic view (A) and narrow band imaging (B). Subsequent colonoscopy after lung transplant showing resolution of polypoid lesion (C).
Disclosures:
Erica Loon indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Speakers Bureau.
Erica Loon, DO1, Mohammad Bilal, MD2. P0263 - Vanishing Act: Colonic Polyps Mimicking Tubular Adenoma Disappear With Resolution of Hypoxia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
