Sunday Poster Session
Category: Colon
P0269 - Polyp Party: Recurrent Clostridium difficile Infection Complicated by Severe Inflammatory Pseudopolyps
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Akira Folk, DO
Banner - University of Arizona
Tucson, AZ
Presenting Author(s)
Akira Folk, DO1, Sean Moore, DO1, Samuel H. Cheong, DO1, Maxwell Hart, MD1, Brandon Witten, MD2, Jaime Scott, MD1, Cameron Thompson, MD1
1Banner - University of Arizona, Tucson, AZ; 2University of Arizona College of Medicine, Tucson, AZ
Introduction: Pseudopolyps are nonmalignant inflammatory growths often forming in the gastrointestinal tract lining in response to severe inflammation, most commonly seen in patients with inflammatory bowel diseases (IBD) such as ulcerative colitis or Crohn’s disease.
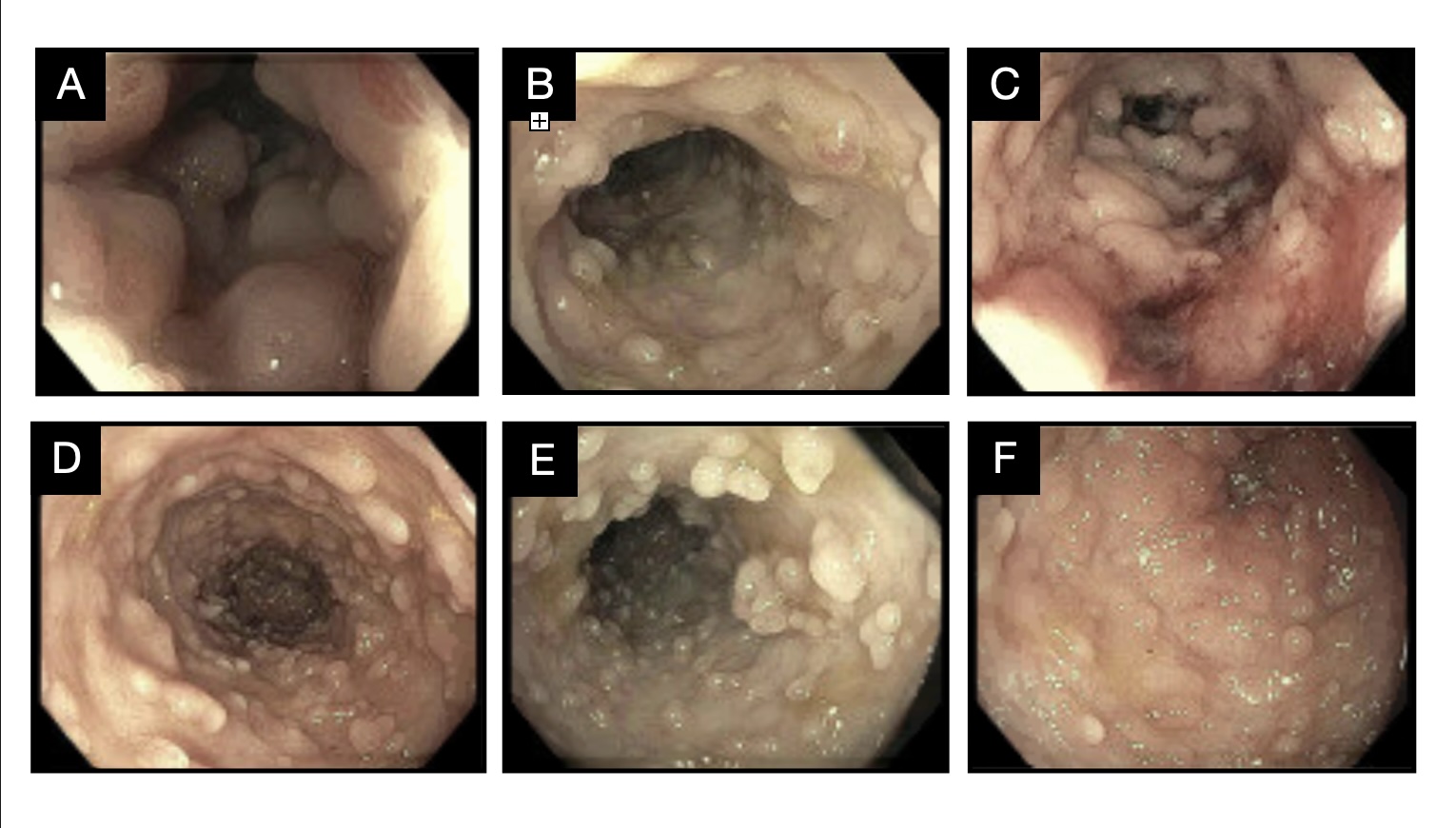
Case Description/Methods: This case report details the complex clinical course of a 66-year-old female with multiple sclerosis (MS) who presented with severe diarrhea attributed to recurrent Clostridium difficile infection (CDI) and was found to have numerous inflammatory pseudopolyps lining her colon. Despite completing oral vancomycin therapy twice after testing positive for CDI complicated by pseudomembranous colitis, the patient returned with daily foul-smelling loose stools and altered mental status. Diagnostic challenges arose as all subsequent CDI tests yielded negative results. After failing to respond to empiric CDI treatment, a colonoscopy revealed thousands of inflammatory pseudopolyps and colonic narrowing, diagnosed as a consequence of recurrent CDI colitis. Biopsies ruled out malignancy, IBD, and microscopic colitis. The patient began a long vancomycin taper, initially showing symptomatic improvement. However, she relapsed within two weeks of discharge. Repeat CDI testing indicated positive antigen but negative PCR results. Her symptoms improved greatly after initiation of Fidaxomicin, and she was scheduled for outpatient fecal microbiota transplantation (FMT).
Discussion: This case contributes to the expanding body of knowledge of CDI, highlighting its intricate and unexpected association with inflammatory pseudopolyps. It is important to acknowledge that high polyp burden can result in narrowing of the colon and present as obstructive-type symptoms. Thus, this case report demonstrates the value of considering diverse clinical presentations for timely and effective patient care. The pathogenesis of CDI, marked by microbial dysbiosis, underscores the need for early microbial-based therapies such as FMT to prevent long-term mucosal injury, particularly in immunocompromised individuals. Continued research in CDI treatment is essential, given the potential for resistance development with potent drugs like vancomycin and fidaxomicin. Considering the overlap in clinical presentations between CDI and IBD, ruling out underlying IBD is crucial for proper management and to prevent misdiagnosis and mistreatment.
Disclosures:
Akira Folk, DO1, Sean Moore, DO1, Samuel H. Cheong, DO1, Maxwell Hart, MD1, Brandon Witten, MD2, Jaime Scott, MD1, Cameron Thompson, MD1. P0269 - Polyp Party: Recurrent <i>Clostridium difficile</i> Infection Complicated by Severe Inflammatory Pseudopolyps, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Banner - University of Arizona, Tucson, AZ; 2University of Arizona College of Medicine, Tucson, AZ
Introduction: Pseudopolyps are nonmalignant inflammatory growths often forming in the gastrointestinal tract lining in response to severe inflammation, most commonly seen in patients with inflammatory bowel diseases (IBD) such as ulcerative colitis or Crohn’s disease.
Case Description/Methods: This case report details the complex clinical course of a 66-year-old female with multiple sclerosis (MS) who presented with severe diarrhea attributed to recurrent Clostridium difficile infection (CDI) and was found to have numerous inflammatory pseudopolyps lining her colon. Despite completing oral vancomycin therapy twice after testing positive for CDI complicated by pseudomembranous colitis, the patient returned with daily foul-smelling loose stools and altered mental status. Diagnostic challenges arose as all subsequent CDI tests yielded negative results. After failing to respond to empiric CDI treatment, a colonoscopy revealed thousands of inflammatory pseudopolyps and colonic narrowing, diagnosed as a consequence of recurrent CDI colitis. Biopsies ruled out malignancy, IBD, and microscopic colitis. The patient began a long vancomycin taper, initially showing symptomatic improvement. However, she relapsed within two weeks of discharge. Repeat CDI testing indicated positive antigen but negative PCR results. Her symptoms improved greatly after initiation of Fidaxomicin, and she was scheduled for outpatient fecal microbiota transplantation (FMT).
Discussion: This case contributes to the expanding body of knowledge of CDI, highlighting its intricate and unexpected association with inflammatory pseudopolyps. It is important to acknowledge that high polyp burden can result in narrowing of the colon and present as obstructive-type symptoms. Thus, this case report demonstrates the value of considering diverse clinical presentations for timely and effective patient care. The pathogenesis of CDI, marked by microbial dysbiosis, underscores the need for early microbial-based therapies such as FMT to prevent long-term mucosal injury, particularly in immunocompromised individuals. Continued research in CDI treatment is essential, given the potential for resistance development with potent drugs like vancomycin and fidaxomicin. Considering the overlap in clinical presentations between CDI and IBD, ruling out underlying IBD is crucial for proper management and to prevent misdiagnosis and mistreatment.
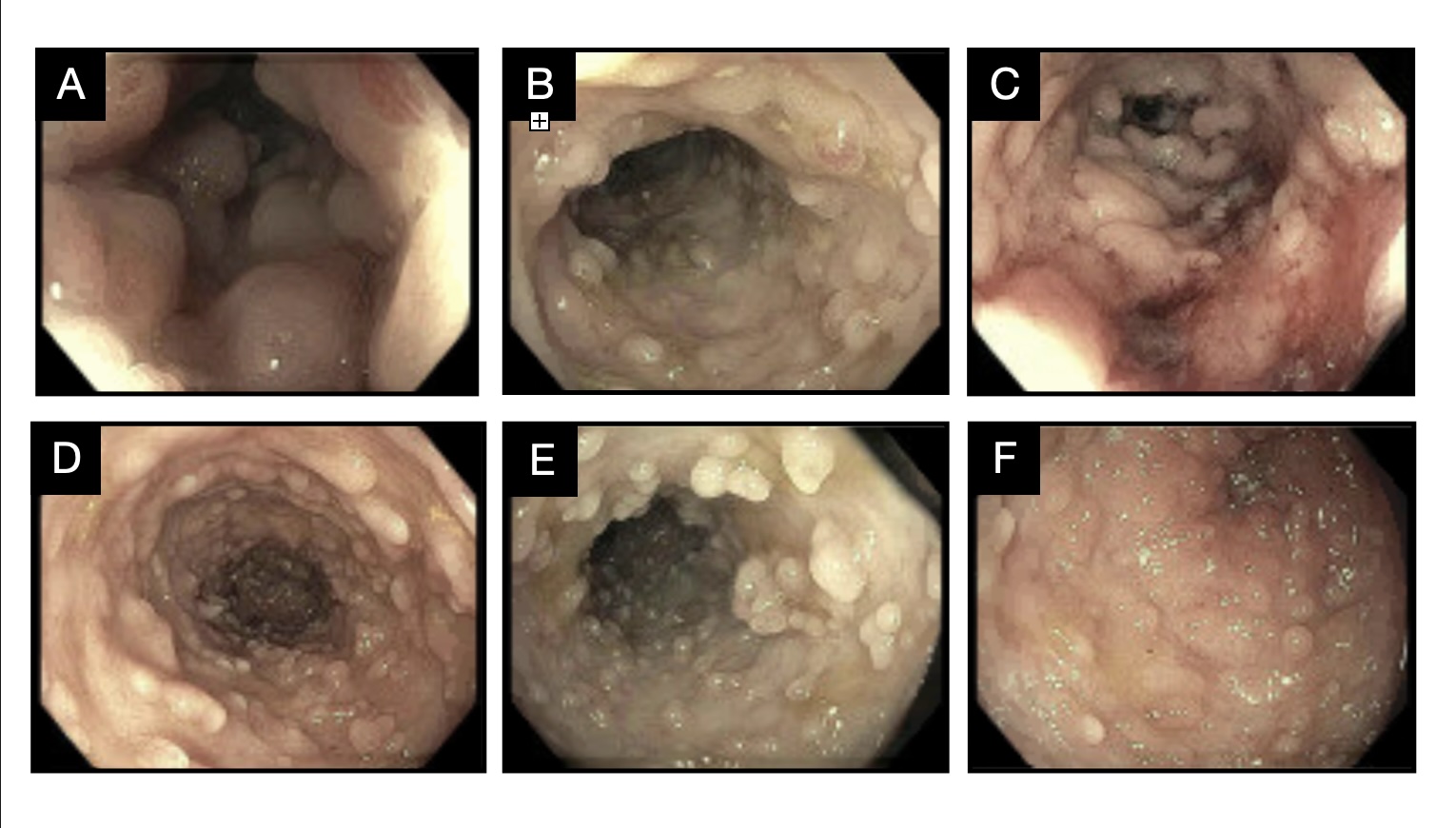
Figure: Figure 1. A-C: Descending colon. D: Splenic flexure. E-F: Transverse colon
Disclosures:
Akira Folk indicated no relevant financial relationships.
Sean Moore indicated no relevant financial relationships.
Samuel Cheong indicated no relevant financial relationships.
Maxwell Hart indicated no relevant financial relationships.
Brandon Witten indicated no relevant financial relationships.
Jaime Scott indicated no relevant financial relationships.
Cameron Thompson indicated no relevant financial relationships.
Akira Folk, DO1, Sean Moore, DO1, Samuel H. Cheong, DO1, Maxwell Hart, MD1, Brandon Witten, MD2, Jaime Scott, MD1, Cameron Thompson, MD1. P0269 - Polyp Party: Recurrent <i>Clostridium difficile</i> Infection Complicated by Severe Inflammatory Pseudopolyps, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
