Sunday Poster Session
Category: Biliary/Pancreas
P0182 - A Case of Obstructive Hepatolithiasis With Hepatic Duct Stricture
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Julia Janecki, DO, MSPH
McLaren Macomb Hospital
Mt. Clemens, MI
Presenting Author(s)
Julia Janecki, DO, MSPH, Abby Kunitsky, DO, Colin Leffert, DO
McLaren Macomb Hospital, Mt. Clemens, MI
Introduction: Hepatolithiasis, or intrahepatic calculi, is the presence of calculi in all bile ducts peripheral to the confluence of the right and left hepatic ducts. Management may require percutaneous transhepatic cholangioscopic lithotomy (PTCSL) or hepatectomy. Here we present a case of a large obstructive intrahepatic calculus and hepatic stricture requiring complex endoscopic intervention.
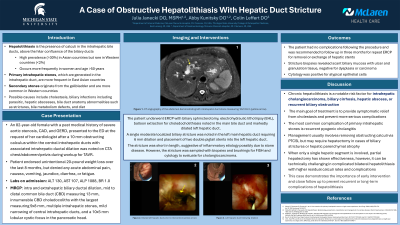
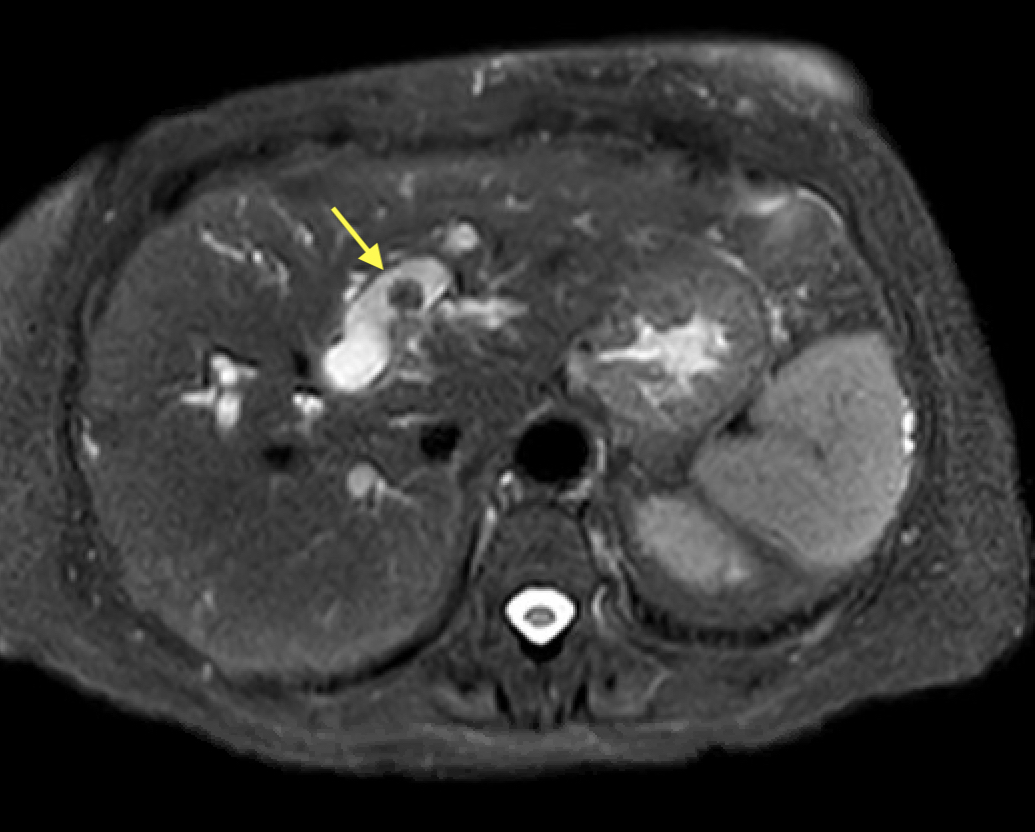
Case Description/Methods: An 82-year-old female with a history of severe aortic stenosis presented to the emergency department after a 10 mm obstructing calculus within the central intrahepatic duct with associated ductal dilation was noted on computed tomography (CT) angiography of the chest/abdomen/pelvis during workup for transcatheter aortic valve replacement. On admission, the patient endorsed mild right upper quadrant pain and unintentional 20-pound weight loss over the past eight months. She denied any vomiting, jaundice, or diarrhea. Labs revealed ALT 130, AST 107, ALP 1088, and total bilirubin of 1.0. Magnetic resonance cholangiopancreatography (MRCP) was performed and revealed intra and extrahepatic biliary ductal dilation, innumerable common bile duct and intrahepatic calculi, mild narrowing of central intrahepatic ducts, and a 10x5 mm lobular cyst in the pancreatic head (Figure 1). Endoscopic retrograde cholangiopancreatography (ERCP) with SpyGlass cholangioscopy was performed and required biliary sphincterotomy with electrohydraulic lithotripsy and balloon extraction for choledocolithiasis noted in the main bile duct and left hepatic duct. Additionally, a single moderate biliary stricture in the left main hepatic duct required 6 mm dilation and placement of two double pigtail stents. The patient had no complications following the procedure and was recommended to follow up in three months for repeat ERCP for stent evaluation.
Discussion: The main goal of treatment for hepatolithiasis is to provide symptomatic relief from cholestasis and prevent more serious complications. Chronic hepatolithiasis is a notable risk factor for intrahepatic cholangiocarcinoma, hepatic abscess, and recurrent biliary obstruction. The most frequent complication of primary intrahepatic stones is recurrent pyogenic cholangitis. Management usually involves removing obstructing calculi via PTCSL, but may require hepatectomy in cases of biliary strictures or hepatic parenchymal atrophy. This case demonstrates the importance of early intervention and close follow up to prevent recurrent or long-term complications of hepatolithiasis.
Disclosures:
Julia Janecki, DO, MSPH, Abby Kunitsky, DO, Colin Leffert, DO. P0182 - A Case of Obstructive Hepatolithiasis With Hepatic Duct Stricture, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
McLaren Macomb Hospital, Mt. Clemens, MI
Introduction: Hepatolithiasis, or intrahepatic calculi, is the presence of calculi in all bile ducts peripheral to the confluence of the right and left hepatic ducts. Management may require percutaneous transhepatic cholangioscopic lithotomy (PTCSL) or hepatectomy. Here we present a case of a large obstructive intrahepatic calculus and hepatic stricture requiring complex endoscopic intervention.
Case Description/Methods: An 82-year-old female with a history of severe aortic stenosis presented to the emergency department after a 10 mm obstructing calculus within the central intrahepatic duct with associated ductal dilation was noted on computed tomography (CT) angiography of the chest/abdomen/pelvis during workup for transcatheter aortic valve replacement. On admission, the patient endorsed mild right upper quadrant pain and unintentional 20-pound weight loss over the past eight months. She denied any vomiting, jaundice, or diarrhea. Labs revealed ALT 130, AST 107, ALP 1088, and total bilirubin of 1.0. Magnetic resonance cholangiopancreatography (MRCP) was performed and revealed intra and extrahepatic biliary ductal dilation, innumerable common bile duct and intrahepatic calculi, mild narrowing of central intrahepatic ducts, and a 10x5 mm lobular cyst in the pancreatic head (Figure 1). Endoscopic retrograde cholangiopancreatography (ERCP) with SpyGlass cholangioscopy was performed and required biliary sphincterotomy with electrohydraulic lithotripsy and balloon extraction for choledocolithiasis noted in the main bile duct and left hepatic duct. Additionally, a single moderate biliary stricture in the left main hepatic duct required 6 mm dilation and placement of two double pigtail stents. The patient had no complications following the procedure and was recommended to follow up in three months for repeat ERCP for stent evaluation.
Discussion: The main goal of treatment for hepatolithiasis is to provide symptomatic relief from cholestasis and prevent more serious complications. Chronic hepatolithiasis is a notable risk factor for intrahepatic cholangiocarcinoma, hepatic abscess, and recurrent biliary obstruction. The most frequent complication of primary intrahepatic stones is recurrent pyogenic cholangitis. Management usually involves removing obstructing calculi via PTCSL, but may require hepatectomy in cases of biliary strictures or hepatic parenchymal atrophy. This case demonstrates the importance of early intervention and close follow up to prevent recurrent or long-term complications of hepatolithiasis.
Figure: Figure 1. Left intrahepatic duct stone measuring 10x10mm (arrow).
Disclosures:
Julia Janecki indicated no relevant financial relationships.
Abby Kunitsky indicated no relevant financial relationships.
Colin Leffert indicated no relevant financial relationships.
Julia Janecki, DO, MSPH, Abby Kunitsky, DO, Colin Leffert, DO. P0182 - A Case of Obstructive Hepatolithiasis With Hepatic Duct Stricture, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

