Sunday Poster Session
Category: Biliary/Pancreas
P0185 - Stent in Stuck Stent to Retrieve an Embedded Uncovered Self-Expandable Metal Stent
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

David Braun, MD
Methodist Dallas Medical Center
Dallas, TX
Presenting Author(s)
David Salus Braun, MD, Kyle Schneider, MD, Paul Tarnasky, MD, FACG
Methodist Dallas Medical Center, Dallas, TX
Introduction: Fully covered self-expandable metal stents (FCSEMS) have become the mainstay of treatment for benign biliary conditions; endoscopic FCSEMS removal can be achieved with relative ease using rat tooth forceps (RTF) or snare. Uncovered self-expandable metal stents (USEMS) are not intended for removal as they become embedded in tissue and are therefore used exclusively for the palliation of malignant obstruction in patients with limited life expectancy. The aim of this report is to expand on the stent-in-stent technique (SIST) that can be utilized for the rare cases in which USEMS extraction is desired.
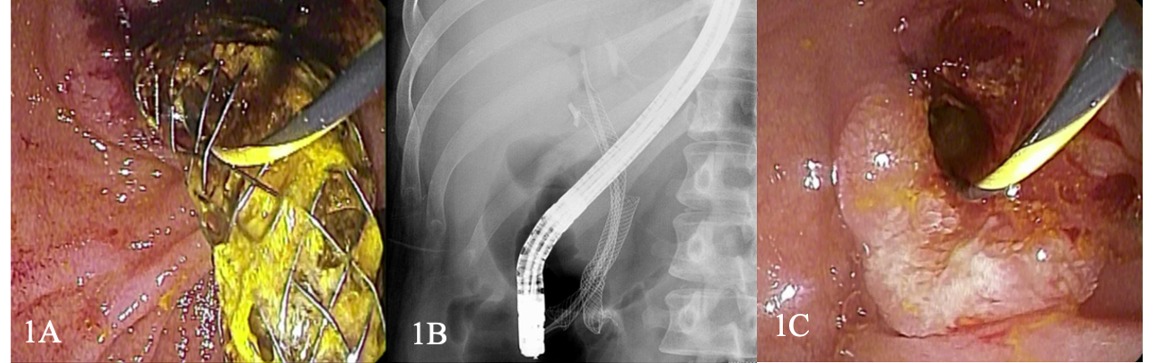
Case Description/Methods: A 27-year-old female was evaluated for right upper quadrant abdominal pain and elevated liver function tests (LFTs). History was significant for cholangitis treated a year earlier with endoscopic retrograde cholangiopancreatography (ERCP) with biliary sphincterotomy and extraction of pus and stones at an outside hospital. A 10 mm x 6 mm FCSEMS was reportedly placed without clear indication. She underwent an uncomplicated cholecystectomy but subsequently was lost to follow up. Physical exam revealed normal vital signs and abdominal tenderness. LFTs yielded elevated total bilirubin 1.3 mg/dL, AST 584 U/L, ALT 775 U/L, ALP 321 U/L; leukocyte count was 9.1 (x 103 U/L). Computed tomography showed a normal liver with a biliary stent in place. ERCP revealed an occluded SEMS. Attempts at stent removal via direct grasping with RTF failed and it became obvious that the stent was an USEMS. The bile duct was cannulated through the interstices of the USEMS (Fig 1A). A 10 mm x 8 cm FCSEMS was placed through the lumen of the USEMS with the intention of inducing pressure necrosis, thereby freeing the embedded stent and facilitating removal at follow up (Fig 1B). Her symptoms resolved promptly after ERCP and LFTs were within normal limits one month later. At repeat ERCP, the FCSEMS was removed without difficulty using RTF (Fig 1C). The patient has remained asymptomatic since stent removal and has not required further intervention.
Discussion: This case highlights the importance of distinguishing between FCSEMS and USEMS prior to stent placement. There are only two other documented cases of successful USEMS removal using SIST. USEMS are not stocked in our ERCP suite. To ensure that intent is for USEMS placement, staff are required to retrieve stock from a separate room when needed. Systems to minimize the erroneous placement of USEMS should be instituted in all endoscopy labs.
Disclosures:
David Salus Braun, MD, Kyle Schneider, MD, Paul Tarnasky, MD, FACG. P0185 - Stent in Stuck Stent to Retrieve an Embedded Uncovered Self-Expandable Metal Stent, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Methodist Dallas Medical Center, Dallas, TX
Introduction: Fully covered self-expandable metal stents (FCSEMS) have become the mainstay of treatment for benign biliary conditions; endoscopic FCSEMS removal can be achieved with relative ease using rat tooth forceps (RTF) or snare. Uncovered self-expandable metal stents (USEMS) are not intended for removal as they become embedded in tissue and are therefore used exclusively for the palliation of malignant obstruction in patients with limited life expectancy. The aim of this report is to expand on the stent-in-stent technique (SIST) that can be utilized for the rare cases in which USEMS extraction is desired.
Case Description/Methods: A 27-year-old female was evaluated for right upper quadrant abdominal pain and elevated liver function tests (LFTs). History was significant for cholangitis treated a year earlier with endoscopic retrograde cholangiopancreatography (ERCP) with biliary sphincterotomy and extraction of pus and stones at an outside hospital. A 10 mm x 6 mm FCSEMS was reportedly placed without clear indication. She underwent an uncomplicated cholecystectomy but subsequently was lost to follow up. Physical exam revealed normal vital signs and abdominal tenderness. LFTs yielded elevated total bilirubin 1.3 mg/dL, AST 584 U/L, ALT 775 U/L, ALP 321 U/L; leukocyte count was 9.1 (x 103 U/L). Computed tomography showed a normal liver with a biliary stent in place. ERCP revealed an occluded SEMS. Attempts at stent removal via direct grasping with RTF failed and it became obvious that the stent was an USEMS. The bile duct was cannulated through the interstices of the USEMS (Fig 1A). A 10 mm x 8 cm FCSEMS was placed through the lumen of the USEMS with the intention of inducing pressure necrosis, thereby freeing the embedded stent and facilitating removal at follow up (Fig 1B). Her symptoms resolved promptly after ERCP and LFTs were within normal limits one month later. At repeat ERCP, the FCSEMS was removed without difficulty using RTF (Fig 1C). The patient has remained asymptomatic since stent removal and has not required further intervention.
Discussion: This case highlights the importance of distinguishing between FCSEMS and USEMS prior to stent placement. There are only two other documented cases of successful USEMS removal using SIST. USEMS are not stocked in our ERCP suite. To ensure that intent is for USEMS placement, staff are required to retrieve stock from a separate room when needed. Systems to minimize the erroneous placement of USEMS should be instituted in all endoscopy labs.
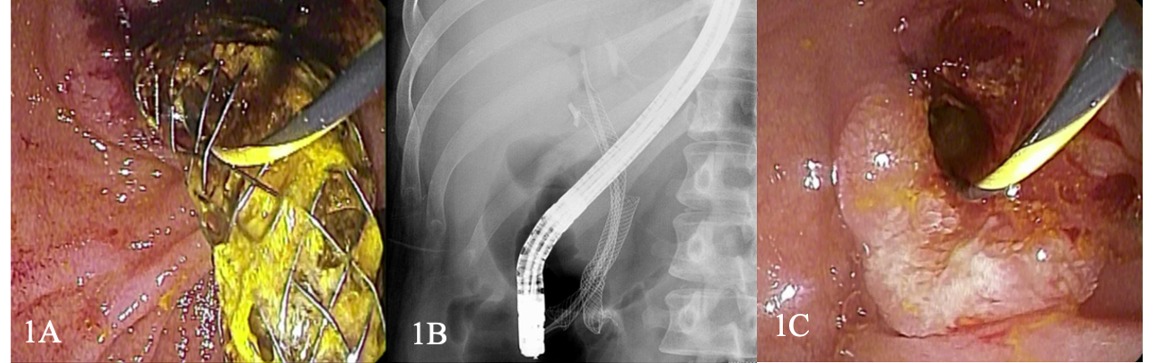
Figure: Fig 1. (A) Endoscopic view of biliary cannulation through the interstices of the uncovered self-expandable metal stent and (B) Fluoroscopic view of fully self-expandable metal stent deployed within uncovered self-expandable metal stent (i.e. stent-in-stent technique) and (C) Endoscopic view of the bile duct after stent removal.
Disclosures:
David Salus Braun indicated no relevant financial relationships.
Kyle Schneider indicated no relevant financial relationships.
Paul Tarnasky indicated no relevant financial relationships.
David Salus Braun, MD, Kyle Schneider, MD, Paul Tarnasky, MD, FACG. P0185 - Stent in Stuck Stent to Retrieve an Embedded Uncovered Self-Expandable Metal Stent, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
