Sunday Poster Session
Category: Biliary/Pancreas
P0189 - Choledocholithiasis Causing Mesenteric Ischemia: A Case Report
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- KE
Kathryn Evey, DO
Brown University / Rhode Island Hospital
Providence, RI
Presenting Author(s)
Kathryn Evey, DO1, Yousef Elfanagely, MD2, Naveena P. Sunkara, MD3, Sean Fine, MD4
1Brown University / Rhode Island Hospital, Providence, RI; 2Brown University, Providence, RI; 3Warren Alpert Medical School of Medicine, Providence, RI; 4Brown Medicine/Brown Physicians, Inc., Providence, RI
Introduction: Mesenteric ischemia (MI) is an inflammatory process of the small bowel due to decreased or interrupted blood flow. Arterial obstruction, venous thromboembolism or low-flow states result in visceral inflammation, edema and tissue ulceration. Without resolution, the mucosa can infarct and lead to death [1]. While MI is rare, it has a mortality rate of 60-80% [2],[3],[4]. There are cases of compression of the celiac axis resulting in MI, however, there are no reports of choledocholithiasis as the cause. We present a case where such a process occurred.
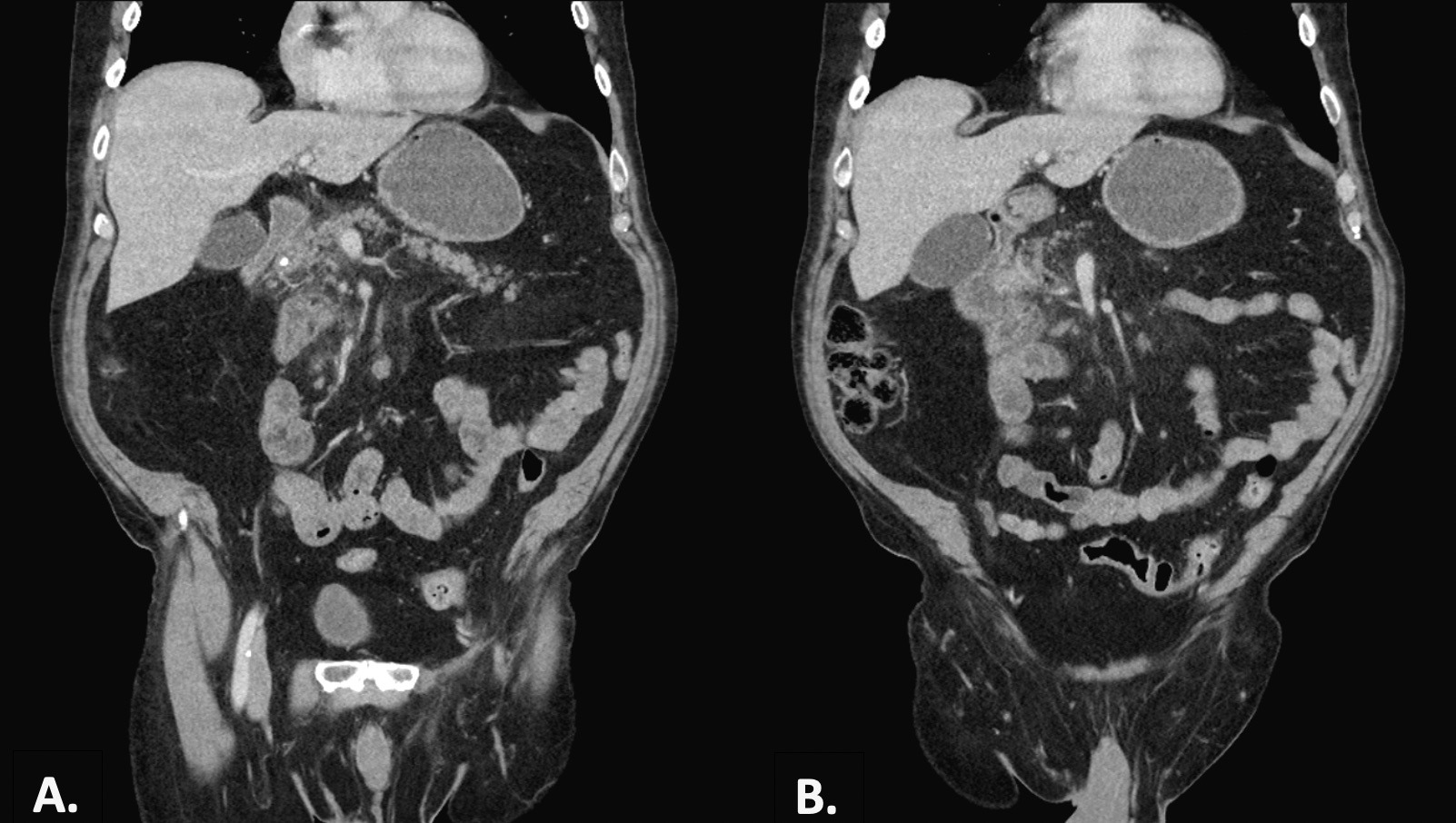
Case Description/Methods: A 76 year-old male with a past medical history of diabetes, hypertension, and hyperlipidemia presented for severe, constant abdominal pain for two weeks. He endorsed bloating, nausea, decreased appetite, constipation, and straining with BM. A colonoscopy two weeks prior was unremarkable. Physical exam noted a distended abdomen with generalized tenderness. Initial labs showed aspartate transaminase (AST) 83 u/L, alanine transaminase (ALT) 296 u/L, alkaline phosphatase 297 u/L, and total bilirubin 1.0 mg/dL. An x-ray revealed dilated loops of small bowel, and a computerized tomography (CT) scan showed wall thickening of a small bowel segment, a non-distended gallbladder, and an enlarged common bile duct (CBD) with multiple distal gallstones. A magnetic resonance cholangiopancreatography (MRCP) confirmed choledocholithiasis. The patient underwent push enteroscopy, and diffuse ulceration and edematous/friable tissue with spontaneous bleeding of the duodenal mucosa was noted. Biopsies were consistent with ischemia. After the procedure, the patient felt relief of pain and distension; and was safely discharged from the hospital.
Discussion: Choledocholithiasis is the presence of gallstones within the CBD that migrated from the gallbladder. Diagnosis relies on clinical symptoms, such as biliary colic or jaundice, and ultrasound, MRCP, or endoscopic retrograde cholangiopancreatography (ERCP) confirmation. Treatment involves endoscopic or surgical stone removal. Typically, choledocholithiasis does not have any impact on the nearby small intestines unless a fistula forms. In this case, however, the anatomic position of the small bowel, adjacent to the CBD, allowed for mechanical compression of the bowel when the duct became dilated. This unprecedented mechanical compression began an inflammatory cascade that would disrupt the oxygen delivery system to the tissue, and result in MI by a mechanism not previously observed in the literature.
Disclosures:
Kathryn Evey, DO1, Yousef Elfanagely, MD2, Naveena P. Sunkara, MD3, Sean Fine, MD4. P0189 - Choledocholithiasis Causing Mesenteric Ischemia: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Brown University / Rhode Island Hospital, Providence, RI; 2Brown University, Providence, RI; 3Warren Alpert Medical School of Medicine, Providence, RI; 4Brown Medicine/Brown Physicians, Inc., Providence, RI
Introduction: Mesenteric ischemia (MI) is an inflammatory process of the small bowel due to decreased or interrupted blood flow. Arterial obstruction, venous thromboembolism or low-flow states result in visceral inflammation, edema and tissue ulceration. Without resolution, the mucosa can infarct and lead to death [1]. While MI is rare, it has a mortality rate of 60-80% [2],[3],[4]. There are cases of compression of the celiac axis resulting in MI, however, there are no reports of choledocholithiasis as the cause. We present a case where such a process occurred.
Case Description/Methods: A 76 year-old male with a past medical history of diabetes, hypertension, and hyperlipidemia presented for severe, constant abdominal pain for two weeks. He endorsed bloating, nausea, decreased appetite, constipation, and straining with BM. A colonoscopy two weeks prior was unremarkable. Physical exam noted a distended abdomen with generalized tenderness. Initial labs showed aspartate transaminase (AST) 83 u/L, alanine transaminase (ALT) 296 u/L, alkaline phosphatase 297 u/L, and total bilirubin 1.0 mg/dL. An x-ray revealed dilated loops of small bowel, and a computerized tomography (CT) scan showed wall thickening of a small bowel segment, a non-distended gallbladder, and an enlarged common bile duct (CBD) with multiple distal gallstones. A magnetic resonance cholangiopancreatography (MRCP) confirmed choledocholithiasis. The patient underwent push enteroscopy, and diffuse ulceration and edematous/friable tissue with spontaneous bleeding of the duodenal mucosa was noted. Biopsies were consistent with ischemia. After the procedure, the patient felt relief of pain and distension; and was safely discharged from the hospital.
Discussion: Choledocholithiasis is the presence of gallstones within the CBD that migrated from the gallbladder. Diagnosis relies on clinical symptoms, such as biliary colic or jaundice, and ultrasound, MRCP, or endoscopic retrograde cholangiopancreatography (ERCP) confirmation. Treatment involves endoscopic or surgical stone removal. Typically, choledocholithiasis does not have any impact on the nearby small intestines unless a fistula forms. In this case, however, the anatomic position of the small bowel, adjacent to the CBD, allowed for mechanical compression of the bowel when the duct became dilated. This unprecedented mechanical compression began an inflammatory cascade that would disrupt the oxygen delivery system to the tissue, and result in MI by a mechanism not previously observed in the literature.
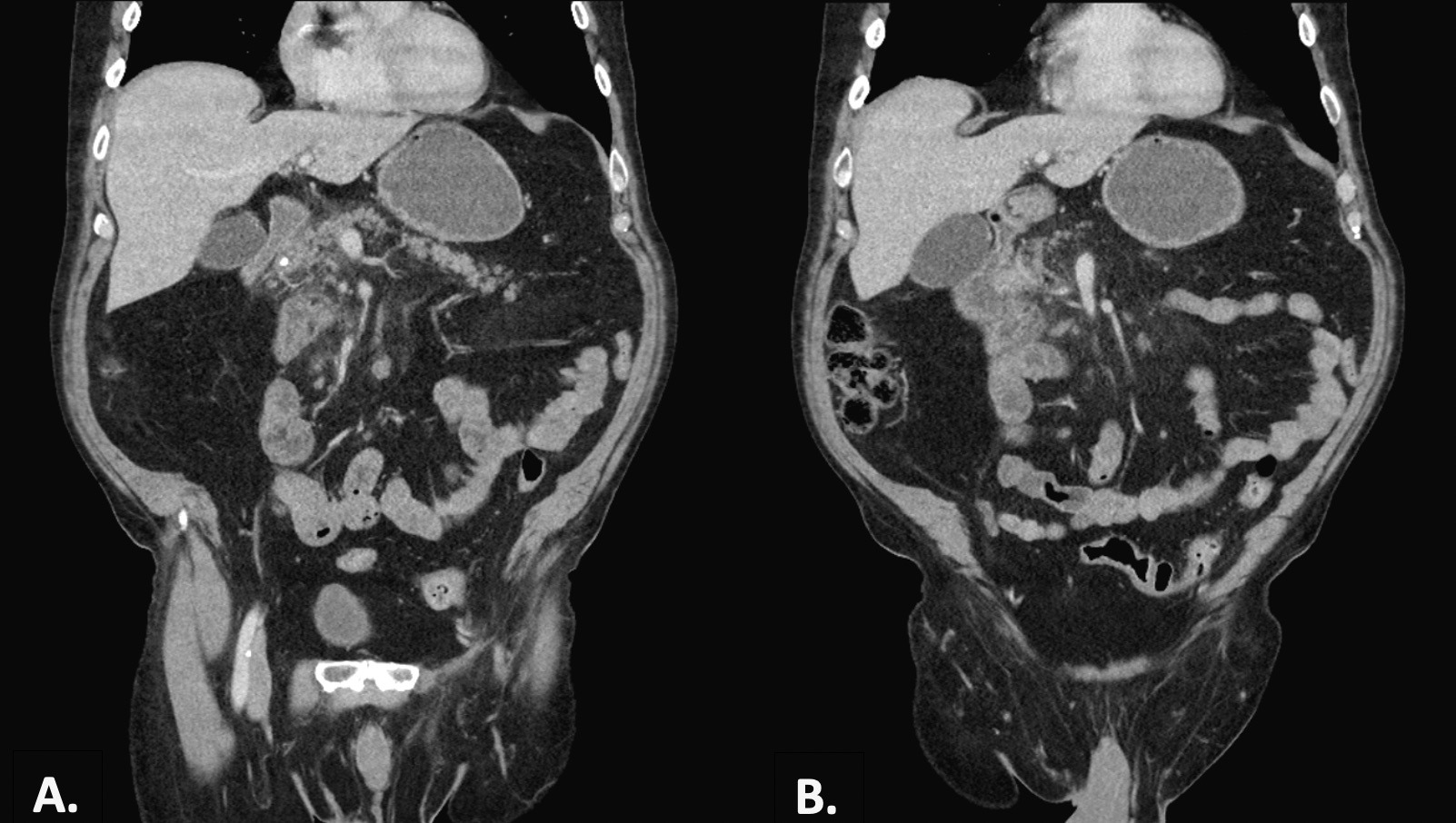
Figure: Figure 1. A. A coronal CT abdomen and pelvis slice that highlights the proximity of the gallstone-containing CBD to the non-rotated duodenum. B. A second slice from the same CT that reveals inflammatory stranding around the duodenum, consistent with mesenteric ischemia.
Disclosures:
Kathryn Evey indicated no relevant financial relationships.
Yousef Elfanagely indicated no relevant financial relationships.
Naveena Sunkara indicated no relevant financial relationships.
Sean Fine: Abbvie – Advisory Committee/Board Member. Jansen – Consultant.
Kathryn Evey, DO1, Yousef Elfanagely, MD2, Naveena P. Sunkara, MD3, Sean Fine, MD4. P0189 - Choledocholithiasis Causing Mesenteric Ischemia: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

