Sunday Poster Session
Category: Biliary/Pancreas
P0199 - Negative Does Not Mean No: Exercising Persistence in the Evaluation of a Pancreatic Neuroendocrine Tumor
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- ML
Muhddesa Lakhana, DO
Mount Sinai South Nassau, Icahn School of Medicine at Mount Sinai
Oceanside, NY
Presenting Author(s)
Muhddesa Lakhana, DO1, Rama Hussein, DO2, Marni H. Wilkoff, DO3, Rashmi Advani, MD1
1Mount Sinai South Nassau, Icahn School of Medicine at Mount Sinai, Oceanside, NY; 2Mount Sinai Morningside, New York, NY; 3Mount Sinai Morningside/West, New York, NY
Introduction: Well-differentiated pancreatic neuroendocrine tumors (PanNET) account for 1-3% of pancreatic neoplasms. The most common functioning PanNET is an insulinoma. The underlying hypoglycemia associated with insulinomas may contribute to a wide range of symptoms. The presentation of insulinomas include a wide range of neurological and sympathoadrenal symptoms including visual changes, seizures palpitations, diaphoresis and tremulousness. Insulinomas are often diagnosed with imaging, such as computed tomography (CT) scan or magnetic resonance imaging (MRI), with lab work showing high insulin levels. We present a case of a patient who was treated for suspected absence seizures for one year prior to discovering an insulinoma on Endoscopic Ultrasound (EUS), that was undetected on MRI.
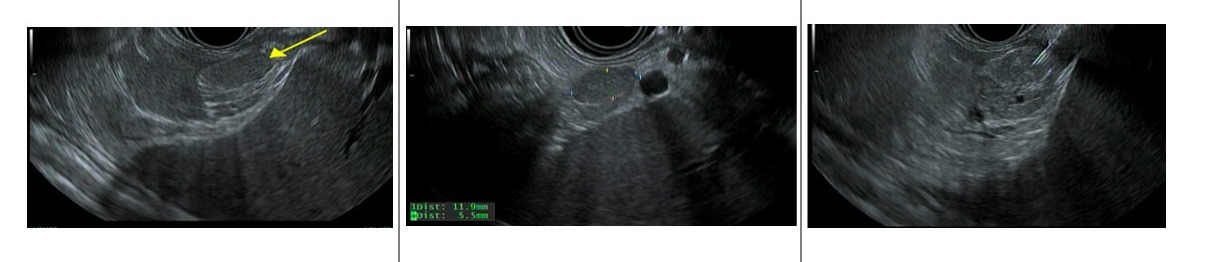
Case Description/Methods: A 29-year-old female was being seen by a Neurologist for one year of episodic disorientation, blurry vision, and unresponsiveness, and was diagnosed with absence seizures. She was placed on anti-epileptic medications, however, despite treatment, her symptoms persisted. Lab testing performed by her Neurologist revealed non-fasting serum glucose levels varying from 32mg/dL to 53mg/dL. The patient was referred to an Endocrinologist who conducted a 72-hour fasting glucose test. Her serum glucose level was 53mg/dL with c-peptide of 3.64mg/dL and a total insulin of 26.3mg/dL. The patient endorsed fatigue during times of hypoglycemia. Follow-up CT abdomen and pelvis and MRI cholangiogram were negative for pancreatobiliary pathology. The patient was referred to Interventional Gastroenterology for EUS, which revealed a 12mm by 6mm well defined, isoechoic and heterogenous lesion within the pancreatic tail. Pathology was consistent with a grade 1 well-differentiated pancreatic neuroendocrine tumor (PanNET).
Discussion: Well-differentiated PanNETs are an uncommon cause of pancreatic neoplasms and are further divided into functioning and nonfunctioning tumors. Of the functioning tumors, about 30-35% are insulinomas, where patients produce excess insulin resulting in low blood glucose (< 50mg/dL) and may manifest with symptoms such as blurry vision, diaphoresis and even seizures. Both CT scan and MRI have an 89-97% sensitivity. EUS allows for direct visualization as well as biopsy. Our case highlights the importance of maintaining a high degree of suspicion in the face of persistent clinical symptoms despite negative imaging, as EUS was able to diagnose an insulinoma for our patient.
Disclosures:
Muhddesa Lakhana, DO1, Rama Hussein, DO2, Marni H. Wilkoff, DO3, Rashmi Advani, MD1. P0199 - Negative Does Not Mean No: Exercising Persistence in the Evaluation of a Pancreatic Neuroendocrine Tumor, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mount Sinai South Nassau, Icahn School of Medicine at Mount Sinai, Oceanside, NY; 2Mount Sinai Morningside, New York, NY; 3Mount Sinai Morningside/West, New York, NY
Introduction: Well-differentiated pancreatic neuroendocrine tumors (PanNET) account for 1-3% of pancreatic neoplasms. The most common functioning PanNET is an insulinoma. The underlying hypoglycemia associated with insulinomas may contribute to a wide range of symptoms. The presentation of insulinomas include a wide range of neurological and sympathoadrenal symptoms including visual changes, seizures palpitations, diaphoresis and tremulousness. Insulinomas are often diagnosed with imaging, such as computed tomography (CT) scan or magnetic resonance imaging (MRI), with lab work showing high insulin levels. We present a case of a patient who was treated for suspected absence seizures for one year prior to discovering an insulinoma on Endoscopic Ultrasound (EUS), that was undetected on MRI.
Case Description/Methods: A 29-year-old female was being seen by a Neurologist for one year of episodic disorientation, blurry vision, and unresponsiveness, and was diagnosed with absence seizures. She was placed on anti-epileptic medications, however, despite treatment, her symptoms persisted. Lab testing performed by her Neurologist revealed non-fasting serum glucose levels varying from 32mg/dL to 53mg/dL. The patient was referred to an Endocrinologist who conducted a 72-hour fasting glucose test. Her serum glucose level was 53mg/dL with c-peptide of 3.64mg/dL and a total insulin of 26.3mg/dL. The patient endorsed fatigue during times of hypoglycemia. Follow-up CT abdomen and pelvis and MRI cholangiogram were negative for pancreatobiliary pathology. The patient was referred to Interventional Gastroenterology for EUS, which revealed a 12mm by 6mm well defined, isoechoic and heterogenous lesion within the pancreatic tail. Pathology was consistent with a grade 1 well-differentiated pancreatic neuroendocrine tumor (PanNET).
Discussion: Well-differentiated PanNETs are an uncommon cause of pancreatic neoplasms and are further divided into functioning and nonfunctioning tumors. Of the functioning tumors, about 30-35% are insulinomas, where patients produce excess insulin resulting in low blood glucose (< 50mg/dL) and may manifest with symptoms such as blurry vision, diaphoresis and even seizures. Both CT scan and MRI have an 89-97% sensitivity. EUS allows for direct visualization as well as biopsy. Our case highlights the importance of maintaining a high degree of suspicion in the face of persistent clinical symptoms despite negative imaging, as EUS was able to diagnose an insulinoma for our patient.
Figure: Isoechoic mass noted in pancreatic tail.
Disclosures:
Muhddesa Lakhana indicated no relevant financial relationships.
Rama Hussein indicated no relevant financial relationships.
Marni Wilkoff indicated no relevant financial relationships.
Rashmi Advani indicated no relevant financial relationships.
Muhddesa Lakhana, DO1, Rama Hussein, DO2, Marni H. Wilkoff, DO3, Rashmi Advani, MD1. P0199 - Negative Does Not Mean No: Exercising Persistence in the Evaluation of a Pancreatic Neuroendocrine Tumor, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
