Sunday Poster Session
Category: Biliary/Pancreas
P0122 - A Rare Case of Cannabis Induced Pancreatitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- CK
Charitha Karanam Ramapathy, MBBS
Baptist Medical Center South
Montgomery, AL
Presenting Author(s)
Charitha Karanam Ramapathy, MBBS, Rakesh Kanipakam, MD, Binay Kshetree, MD
Baptist Medical Center South, Montgomery, AL
Introduction: Acute pancreatitis(AP)is among the top three leading causes of gastroenterology-related hospitalizations annually in the United States, accounting for approximately 300,000 cases and the associated costs of approximately $2.6 billion. Common reasons include continue to be gallstones, alcohol abuse, smoking, hypertriglyceridemia, infections, trauma, drugs, malignancy, scorpion stings, hypercalcemia, endoscopic retrograde cholangiopancreatography (ERCP) and rarely cannabis along with other drugs. Cannabis exposure has been steadily increasing across the world with United States leading the way mainly after it has been used for variety of medical conditions. It is imperative to understand the impact of cannabis use on one’s health with long term use with increasing usage.
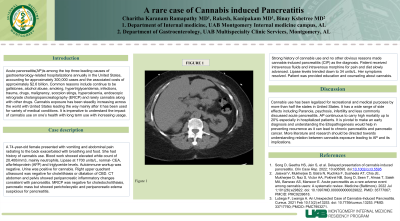
Case Description/Methods: A 74-year-old female presented with vomiting and abdominal pain radiating to the back exacerbated with breathing and food. She had history of cannabis use. Blood work showed elevated white count of 20,400/mm3, mainly neutrophils, Lipase at 1700 units/L, normal- CEA, alfa-fetoprotein (AFP) and triglyceride levels. Autoimmune workup was negative. Urine was positive for cannabis. Right upper quadrant ultrasound was negative for cholelithiasis or dilatation of CBD. CT abdomen and pelvis showed peripancreatic inflammatory changes consistent with pancreatitis. MRCP was negative for choledocholithiasis, pancreatic mass but showed pericholecystic and peripancreatic edema suspicious for pancreatitis. Strong history of cannabis use and no other obvious reasons made cannabis-induced pancreatitis (CIP) as the diagnosis. Patient received intravenous fluids and intravenous morphine for pain and diet slowly advanced. Lipase levels trended down to 34 units/L. Her symptoms resolved. Patient was provided education and counseling about cannabis.
Discussion: Cannabis use has been legalized for recreational and medical purposes by more than half the states in United States. It has a wide range of side effects including Paranoia, psychosis, infertility and less commonly discussed acute pancreatitis. AP continuous to carry high mortality up to 20% especially in hospitalized patients. It is pivotal to make an early diagnosis and understanding the Etiopathogenesis would help in preventing recurrence as it can lead to chronic pancreatitis and pancreatic cancer. More literature and research should be directed towards understanding relation between cannabis exposure leading to AP and its implications.

Disclosures:
Charitha Karanam Ramapathy, MBBS, Rakesh Kanipakam, MD, Binay Kshetree, MD. P0122 - A Rare Case of Cannabis Induced Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Baptist Medical Center South, Montgomery, AL
Introduction: Acute pancreatitis(AP)is among the top three leading causes of gastroenterology-related hospitalizations annually in the United States, accounting for approximately 300,000 cases and the associated costs of approximately $2.6 billion. Common reasons include continue to be gallstones, alcohol abuse, smoking, hypertriglyceridemia, infections, trauma, drugs, malignancy, scorpion stings, hypercalcemia, endoscopic retrograde cholangiopancreatography (ERCP) and rarely cannabis along with other drugs. Cannabis exposure has been steadily increasing across the world with United States leading the way mainly after it has been used for variety of medical conditions. It is imperative to understand the impact of cannabis use on one’s health with long term use with increasing usage.
Case Description/Methods: A 74-year-old female presented with vomiting and abdominal pain radiating to the back exacerbated with breathing and food. She had history of cannabis use. Blood work showed elevated white count of 20,400/mm3, mainly neutrophils, Lipase at 1700 units/L, normal- CEA, alfa-fetoprotein (AFP) and triglyceride levels. Autoimmune workup was negative. Urine was positive for cannabis. Right upper quadrant ultrasound was negative for cholelithiasis or dilatation of CBD. CT abdomen and pelvis showed peripancreatic inflammatory changes consistent with pancreatitis. MRCP was negative for choledocholithiasis, pancreatic mass but showed pericholecystic and peripancreatic edema suspicious for pancreatitis. Strong history of cannabis use and no other obvious reasons made cannabis-induced pancreatitis (CIP) as the diagnosis. Patient received intravenous fluids and intravenous morphine for pain and diet slowly advanced. Lipase levels trended down to 34 units/L. Her symptoms resolved. Patient was provided education and counseling about cannabis.
Discussion: Cannabis use has been legalized for recreational and medical purposes by more than half the states in United States. It has a wide range of side effects including Paranoia, psychosis, infertility and less commonly discussed acute pancreatitis. AP continuous to carry high mortality up to 20% especially in hospitalized patients. It is pivotal to make an early diagnosis and understanding the Etiopathogenesis would help in preventing recurrence as it can lead to chronic pancreatitis and pancreatic cancer. More literature and research should be directed towards understanding relation between cannabis exposure leading to AP and its implications.

Figure: CT abdomen and pelvis showed peripancreatic inflammatory changes consistent with pancreatitis.
Disclosures:
Charitha Karanam Ramapathy indicated no relevant financial relationships.
Rakesh Kanipakam indicated no relevant financial relationships.
Binay Kshetree indicated no relevant financial relationships.
Charitha Karanam Ramapathy, MBBS, Rakesh Kanipakam, MD, Binay Kshetree, MD. P0122 - A Rare Case of Cannabis Induced Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
