Sunday Poster Session
Category: Biliary/Pancreas
P0052 - Sarcopenia is Associated With Increased Mortality And Resource Utilization in Patients With Chronic Pancreatitis: Analysis of National Inpatient Sample 2016-2020
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- AS
Anmol Singh, MBBS
Tristar Centennial Medical Center
Nashville, TN
Presenting Author(s)
Anmol Singh, MBBS1, Sahiljot Bhupal, MBBS2, Carol Singh, MBBS3, Vikash Kumar, MD4, Ritika Dhruve, MBBS5, Aalam Sohal, MD6, Juliana Yang, MD7
1Tristar Centennial Medical Center, Nashville, TN; 2Dayanand Medical College and Hospital, Chicago, IL; 3Dayanand Medical College and Hospital, Jalandhar, Punjab, India; 4Creighton University School of Medicine, Brooklyn, NY; 5University of Texas Southwestern Medical Center, Dallas, TX; 6Creighton University School of Medicine, Seattle, WA; 7University of Texas Medical Branch, Galveston, TX
Introduction: Malnutrition is a common sequela of chronic pancreatitis (CP), which can lead to the development of secondary sarcopenia. Recent studies have suggested that sarcopenia may be associated with adverse outcomes in CP patients. The current study examines the impact of sarcopenia on outcomes in patients with CP.
Methods: We used the National Inpatient Sample 2016-2020 to identify adult patients ( >18 yrs) with CP. Patients were stratified into two groups based on the presence of sarcopenia. Patients with missing demographics or mortality were excluded. Data was collected on patient demographics, hospital characteristics, and comorbidities. The outcomes assessed were in-hospital mortality, sepsis, shock, acute kidney injury and resource utilization. Multivariate regression analysis was used to assess the relationship between sarcopenia and clinical outcomes in patients with chronic pancreatitis.
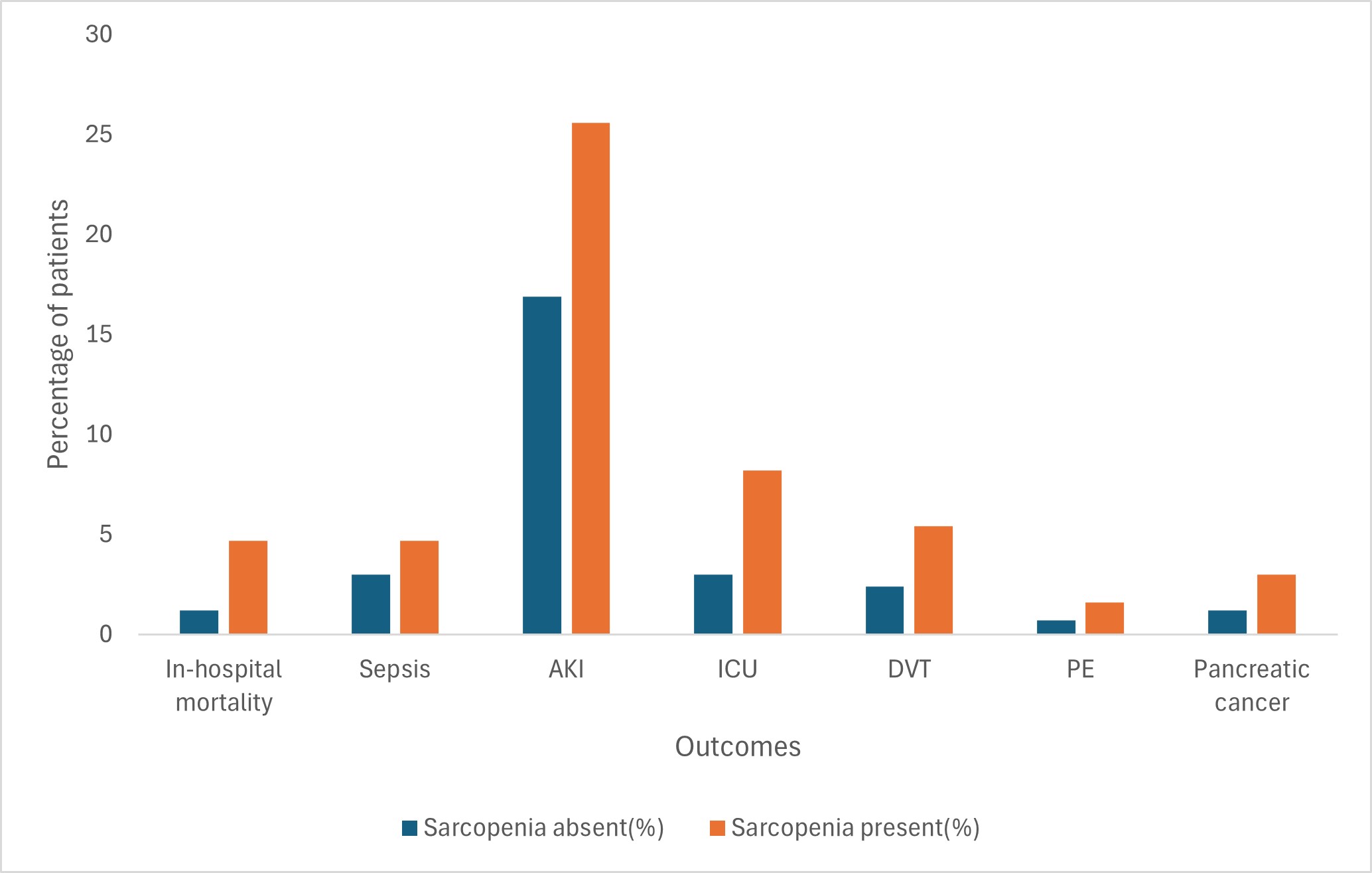
Results: Of 907,790 patients with CP, 165,900 (18.3%) had sarcopenia. The majority of patients with sarcopenia were Male (55.9%), White (65.8%), and had Medicare insurance (44.5%). Patients with sarcopenia had higher in-hospital mortality (4.7% vs. 1.2%,p< 0.001), sepsis (4.7% vs 3%,p< 0.001), AKI (25.6% vs. 16.9%,p< 0.001), ICU admission (8.2% vs. 3%, p< 0.001), deep vein thrombosis (5.4% vs. 2.4%,p< 0.001), pulmonary embolism (1.6 vs 0.7%,p< 0.001) and pancreatic cancer (3% vs. 1.2%, < 0.001). After adjusting for confounding factors, patients with sarcopenia had higher odds of in-hospital mortality (aOR-3.29, 95% CI-3.06-3.54, p< 0.001), sepsis (aOR-1.58, 95% CI-1.49-1.69,p< 0.001), AKI (aOR-1.46, 95% CI-1.42-.1.51,p< 0.001), ICU admission (aOR- 2.6, 95% CI – 2.47-2.74, p< 0.001), deep vein thrombosis (aOR-2.11, 95% CI-1.81-2.16,p< 0.001), pulmonary embolism (aOR-2.19, 95% CI-1.96-2.45,p< 0.001), and pancreatic cancer (aOR- 1.98, 95% CI – 1.81-2.16, p< 0.001). Patients with sarcopenia also had a statistically significant longer length of stay (Adj. coefficient 3.87, 95% CI-3.75-4,p< 0.001) and higher hospitalization charges (Adj. coefficient 40285.15, 95% CI-38,072.5-48,497.75,p< 0.001).
Discussion: Our study reports that patients with sarcopenia are at higher risk of worse outcomes compared to those without sarcopenia. Physicians should be aware of these findings, and early interventions aimed at improving the nutritional status in this high-risk population are warranted.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Anmol Singh, MBBS1, Sahiljot Bhupal, MBBS2, Carol Singh, MBBS3, Vikash Kumar, MD4, Ritika Dhruve, MBBS5, Aalam Sohal, MD6, Juliana Yang, MD7. P0052 - Sarcopenia is Associated With Increased Mortality And Resource Utilization in Patients With Chronic Pancreatitis: Analysis of National Inpatient Sample 2016-2020, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Tristar Centennial Medical Center, Nashville, TN; 2Dayanand Medical College and Hospital, Chicago, IL; 3Dayanand Medical College and Hospital, Jalandhar, Punjab, India; 4Creighton University School of Medicine, Brooklyn, NY; 5University of Texas Southwestern Medical Center, Dallas, TX; 6Creighton University School of Medicine, Seattle, WA; 7University of Texas Medical Branch, Galveston, TX
Introduction: Malnutrition is a common sequela of chronic pancreatitis (CP), which can lead to the development of secondary sarcopenia. Recent studies have suggested that sarcopenia may be associated with adverse outcomes in CP patients. The current study examines the impact of sarcopenia on outcomes in patients with CP.
Methods: We used the National Inpatient Sample 2016-2020 to identify adult patients ( >18 yrs) with CP. Patients were stratified into two groups based on the presence of sarcopenia. Patients with missing demographics or mortality were excluded. Data was collected on patient demographics, hospital characteristics, and comorbidities. The outcomes assessed were in-hospital mortality, sepsis, shock, acute kidney injury and resource utilization. Multivariate regression analysis was used to assess the relationship between sarcopenia and clinical outcomes in patients with chronic pancreatitis.
Results: Of 907,790 patients with CP, 165,900 (18.3%) had sarcopenia. The majority of patients with sarcopenia were Male (55.9%), White (65.8%), and had Medicare insurance (44.5%). Patients with sarcopenia had higher in-hospital mortality (4.7% vs. 1.2%,p< 0.001), sepsis (4.7% vs 3%,p< 0.001), AKI (25.6% vs. 16.9%,p< 0.001), ICU admission (8.2% vs. 3%, p< 0.001), deep vein thrombosis (5.4% vs. 2.4%,p< 0.001), pulmonary embolism (1.6 vs 0.7%,p< 0.001) and pancreatic cancer (3% vs. 1.2%, < 0.001). After adjusting for confounding factors, patients with sarcopenia had higher odds of in-hospital mortality (aOR-3.29, 95% CI-3.06-3.54, p< 0.001), sepsis (aOR-1.58, 95% CI-1.49-1.69,p< 0.001), AKI (aOR-1.46, 95% CI-1.42-.1.51,p< 0.001), ICU admission (aOR- 2.6, 95% CI – 2.47-2.74, p< 0.001), deep vein thrombosis (aOR-2.11, 95% CI-1.81-2.16,p< 0.001), pulmonary embolism (aOR-2.19, 95% CI-1.96-2.45,p< 0.001), and pancreatic cancer (aOR- 1.98, 95% CI – 1.81-2.16, p< 0.001). Patients with sarcopenia also had a statistically significant longer length of stay (Adj. coefficient 3.87, 95% CI-3.75-4,p< 0.001) and higher hospitalization charges (Adj. coefficient 40285.15, 95% CI-38,072.5-48,497.75,p< 0.001).
Discussion: Our study reports that patients with sarcopenia are at higher risk of worse outcomes compared to those without sarcopenia. Physicians should be aware of these findings, and early interventions aimed at improving the nutritional status in this high-risk population are warranted.
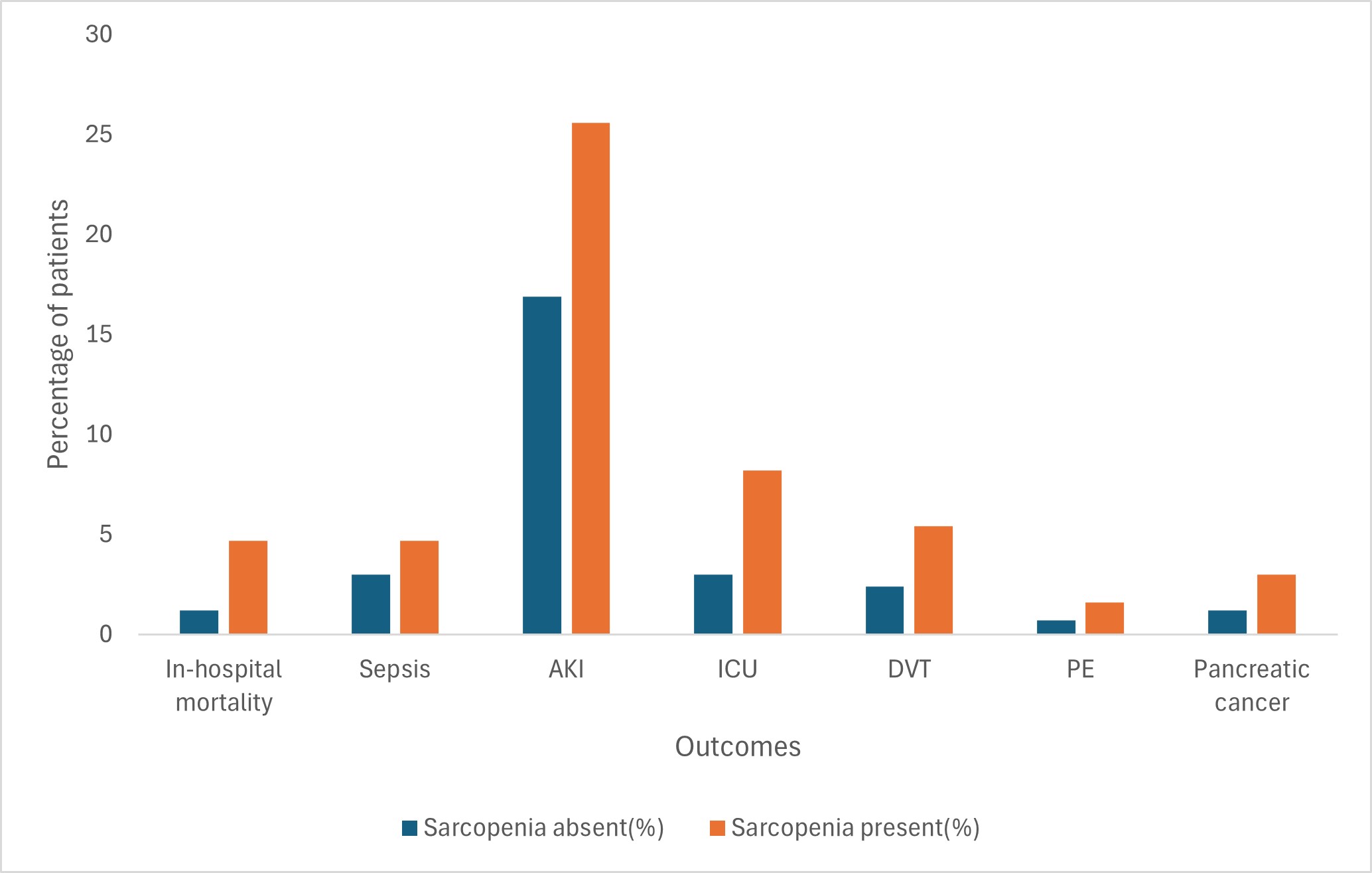
Figure: Clinical outcomes in Chronic pancreatitis patients with and without Sarcopenia
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Anmol Singh indicated no relevant financial relationships.
Sahiljot Bhupal indicated no relevant financial relationships.
Carol Singh indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Ritika Dhruve indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Juliana Yang indicated no relevant financial relationships.
Anmol Singh, MBBS1, Sahiljot Bhupal, MBBS2, Carol Singh, MBBS3, Vikash Kumar, MD4, Ritika Dhruve, MBBS5, Aalam Sohal, MD6, Juliana Yang, MD7. P0052 - Sarcopenia is Associated With Increased Mortality And Resource Utilization in Patients With Chronic Pancreatitis: Analysis of National Inpatient Sample 2016-2020, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
