Sunday Poster Session
Category: Biliary/Pancreas
P0062 - Antibiotic Therapy is Associated with Greater Length of Stay in Mild and Moderate Pancreatitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Neil Gambhir, DO
Lenox Hill Hospital, Northwell Health
New York, NY
Presenting Author(s)
Neil Gambhir, DO1, Dhruv Shankar, MD2, Peter Bhandari, MD1, Samantha Rubin, DO1, Jonathan Jeong, DO1, Jeffrey Dong, MD3, Tasnin Khan, DO1, Aditya Sreenivasan, MD1
1Lenox Hill Hospital, Northwell Health, New York, NY; 2University of Washington, New York, NY; 3Lenox Hill Hospital, Northwell Health, Long Island City, NY
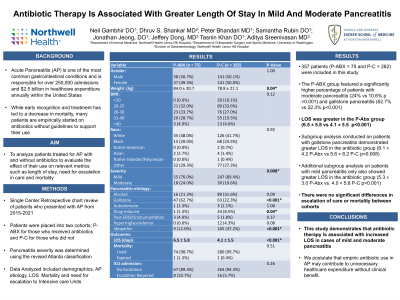
Introduction: Acute Pancreatitis (AP) is one of the most common gastrointestinal conditions and is responsible for over 250,000 admissions and $2.5 billion in healthcare expenditure annually within the United States. While early recognition and treatment has led to a decrease in mortality, many patients are empirically started on antibiotics without guidelines to support their use. This study seeks to analyze patients treated for AP with and without antibiotics to evaluate their effect on relevant metrics such as length of stay (LOS) and mortality.
Methods: Retrospective chart review identified patients who presented with AP from 2015-2021. Patients were placed into two cohorts; P-ABX for those who received antibiotics and P-C for those who did not. Data abstracted included baseline demographics, pancreatitis etiology, LOS, mortality, and escalation of care to intensive care units. Pancreatitis grade (mild/moderate/severe) was determined using the modified Atlanta criterion and patients with severe pancreatitis were excluded. Statistical analysis was conducted and p-values < 0.05 were considered statistically significant.
Results: A total of 357 patients (P-ABX = 75 and P-C = 282) were included in this study (Table 1). The P-ABX group featured a significantly higher percentage of patients with moderate pancreatitis (24% vs 10.6% p <0.001) and gallstone pancreatitis (62.7% vs 22.3% p< 0.001). LOS was greater in the P-ABX group (6.5 ± 5.8 vs 4.1 ± 5.5 p< 0.001). Subgroup analysis conducted on patients with gallstone pancreatitis demonstrated greater LOS in the antibiotic group (6.1 ± 4.2 P-ABX vs 5.6 ± 8.2 P-C p=0.008) with no differences in pancreatitis grade. Additional subgroup analysis on patients with mild pancreatitis only also showed greater LOS in the antibiotic group (5.3 ± 3.0 P-ABX vs. 4.0 ± 5.8 P-C p< 0.001). Overall, there were no significant differences in escalation of care or mortality between cohorts.
Discussion: This study demonstrates that antibiotic therapy is associated with increased LOS in cases of mild and moderate pancreatitis. This association persisted in subgroup analyses of mild pancreatitis and gallstone pancreatitis. In an age of growing antimicrobial resistance and hospital acquired infections, this study indicates that empiric antibiotic use in AP may contribute to unnecessary healthcare expenditure without clinical benefit.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Neil Gambhir, DO1, Dhruv Shankar, MD2, Peter Bhandari, MD1, Samantha Rubin, DO1, Jonathan Jeong, DO1, Jeffrey Dong, MD3, Tasnin Khan, DO1, Aditya Sreenivasan, MD1. P0062 - Antibiotic Therapy is Associated with Greater Length of Stay in Mild and Moderate Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Lenox Hill Hospital, Northwell Health, New York, NY; 2University of Washington, New York, NY; 3Lenox Hill Hospital, Northwell Health, Long Island City, NY
Introduction: Acute Pancreatitis (AP) is one of the most common gastrointestinal conditions and is responsible for over 250,000 admissions and $2.5 billion in healthcare expenditure annually within the United States. While early recognition and treatment has led to a decrease in mortality, many patients are empirically started on antibiotics without guidelines to support their use. This study seeks to analyze patients treated for AP with and without antibiotics to evaluate their effect on relevant metrics such as length of stay (LOS) and mortality.
Methods: Retrospective chart review identified patients who presented with AP from 2015-2021. Patients were placed into two cohorts; P-ABX for those who received antibiotics and P-C for those who did not. Data abstracted included baseline demographics, pancreatitis etiology, LOS, mortality, and escalation of care to intensive care units. Pancreatitis grade (mild/moderate/severe) was determined using the modified Atlanta criterion and patients with severe pancreatitis were excluded. Statistical analysis was conducted and p-values < 0.05 were considered statistically significant.
Results: A total of 357 patients (P-ABX = 75 and P-C = 282) were included in this study (Table 1). The P-ABX group featured a significantly higher percentage of patients with moderate pancreatitis (24% vs 10.6% p <0.001) and gallstone pancreatitis (62.7% vs 22.3% p< 0.001). LOS was greater in the P-ABX group (6.5 ± 5.8 vs 4.1 ± 5.5 p< 0.001). Subgroup analysis conducted on patients with gallstone pancreatitis demonstrated greater LOS in the antibiotic group (6.1 ± 4.2 P-ABX vs 5.6 ± 8.2 P-C p=0.008) with no differences in pancreatitis grade. Additional subgroup analysis on patients with mild pancreatitis only also showed greater LOS in the antibiotic group (5.3 ± 3.0 P-ABX vs. 4.0 ± 5.8 P-C p< 0.001). Overall, there were no significant differences in escalation of care or mortality between cohorts.
Discussion: This study demonstrates that antibiotic therapy is associated with increased LOS in cases of mild and moderate pancreatitis. This association persisted in subgroup analyses of mild pancreatitis and gallstone pancreatitis. In an age of growing antimicrobial resistance and hospital acquired infections, this study indicates that empiric antibiotic use in AP may contribute to unnecessary healthcare expenditure without clinical benefit.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Neil Gambhir indicated no relevant financial relationships.
Dhruv Shankar indicated no relevant financial relationships.
Peter Bhandari indicated no relevant financial relationships.
Samantha Rubin indicated no relevant financial relationships.
Jonathan Jeong indicated no relevant financial relationships.
Jeffrey Dong indicated no relevant financial relationships.
Tasnin Khan indicated no relevant financial relationships.
Aditya Sreenivasan indicated no relevant financial relationships.
Neil Gambhir, DO1, Dhruv Shankar, MD2, Peter Bhandari, MD1, Samantha Rubin, DO1, Jonathan Jeong, DO1, Jeffrey Dong, MD3, Tasnin Khan, DO1, Aditya Sreenivasan, MD1. P0062 - Antibiotic Therapy is Associated with Greater Length of Stay in Mild and Moderate Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
