Sunday Poster Session
Category: Biliary/Pancreas
P0064 - Effect of Positive Intraoperative Cholangiogram on the Rates of Post Endoscopic Retrograde Cholangiopancreatography (ERCP) Pancreatitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Isabelle Nguyen, MD
Scripps Health
La Jolla, CA
Presenting Author(s)
Isabelle Nguyen, MD1, David Leung, MD2, Leah Puglisi, MS3, Franklin Tsai, MD2, Walter Coyle, MD2
1Scripps Health, La Jolla, CA; 2Scripps Green Hospital, La Jolla, CA; 3Scripps Research, La Jolla, CA
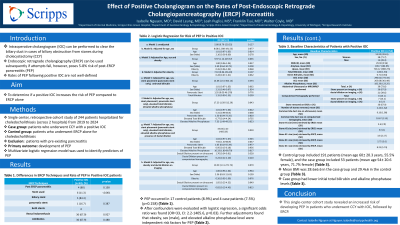
Introduction: In cases of suspected biliary obstruction from stones during cholecystectomy (CCY) for symptomatic cholelithiasis, an intraoperative cholangiogram (IOC) can be performed for diagnosis. If stones are detected, efforts are made to clear the biliary duct through various techniques, such as aggressive duct flushing or glucagon. Patients are referred for endoscopic retrograde cholangiopancreatography (ERCP) if these attempts fail. Post-ERCP pancreatitis (PEP) has a known risk of 5-8%, and it is theorized that attempts to clear stones during the IOC may increase this risk by inadvertent impaction of the stone at the papilla, injury to the papilla, or injecting contrast into the pancreatic duct. The rates for PEP following a positive IOC have not been previously well-defined. The study aimed to determine if a positive IOC increases the risk of PEP compared to ERCP alone.
Methods: We performed a retrospective cohort study of 244 patients hospitalized for choledocholithiasis at a single center (across 2 hospitals) from 2019 to 2024. The case group included patients who underwent CCY with a positive IOC, while the control group comprised patients who underwent ERCP alone for choledocholithiasis. Patients with pancreatitis, including gallstone pancreatitis, at admission were excluded. PEP was defined as abdominal pain within 7 days of ERCP, plus either lipase ≥3 times the upper limit of normal or imaging consistent with pancreatitis. The primary outcome was PEP. A multivariate logistic regression model was used to identify predictors of PEP.
Results: The control group included 191 patients (mean age 60±20.3 years, 55.5% female), and the case group included 53 patients (mean age 54±20.6 years, 71.7% female). The mean BMI was 28.6±6.6 in the case group and 29.4±6 in the control group. The case group had lower initial total bilirubin and alkaline phosphatase levels. PEP occurred in 17 control patients (8.9%) and 4 case patients (7.5%) (p=0.158). After confounders were evaluated with logistic regression, a significant odds ratio was found (OR=33, CI: 2.2-1405.6, p=0.03). Further adjustments found that obesity, sex (male), and elevated alkaline phosphatase level were independent risk factors for PEP (Table 1).
Discussion: This single-center cohort study revealed an increased risk of developing PEP in patients who underwent CCY with IOC, followed by ERCP.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Isabelle Nguyen, MD1, David Leung, MD2, Leah Puglisi, MS3, Franklin Tsai, MD2, Walter Coyle, MD2. P0064 - Effect of Positive Intraoperative Cholangiogram on the Rates of Post Endoscopic Retrograde Cholangiopancreatography (ERCP) Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Scripps Health, La Jolla, CA; 2Scripps Green Hospital, La Jolla, CA; 3Scripps Research, La Jolla, CA
Introduction: In cases of suspected biliary obstruction from stones during cholecystectomy (CCY) for symptomatic cholelithiasis, an intraoperative cholangiogram (IOC) can be performed for diagnosis. If stones are detected, efforts are made to clear the biliary duct through various techniques, such as aggressive duct flushing or glucagon. Patients are referred for endoscopic retrograde cholangiopancreatography (ERCP) if these attempts fail. Post-ERCP pancreatitis (PEP) has a known risk of 5-8%, and it is theorized that attempts to clear stones during the IOC may increase this risk by inadvertent impaction of the stone at the papilla, injury to the papilla, or injecting contrast into the pancreatic duct. The rates for PEP following a positive IOC have not been previously well-defined. The study aimed to determine if a positive IOC increases the risk of PEP compared to ERCP alone.
Methods: We performed a retrospective cohort study of 244 patients hospitalized for choledocholithiasis at a single center (across 2 hospitals) from 2019 to 2024. The case group included patients who underwent CCY with a positive IOC, while the control group comprised patients who underwent ERCP alone for choledocholithiasis. Patients with pancreatitis, including gallstone pancreatitis, at admission were excluded. PEP was defined as abdominal pain within 7 days of ERCP, plus either lipase ≥3 times the upper limit of normal or imaging consistent with pancreatitis. The primary outcome was PEP. A multivariate logistic regression model was used to identify predictors of PEP.
Results: The control group included 191 patients (mean age 60±20.3 years, 55.5% female), and the case group included 53 patients (mean age 54±20.6 years, 71.7% female). The mean BMI was 28.6±6.6 in the case group and 29.4±6 in the control group. The case group had lower initial total bilirubin and alkaline phosphatase levels. PEP occurred in 17 control patients (8.9%) and 4 case patients (7.5%) (p=0.158). After confounders were evaluated with logistic regression, a significant odds ratio was found (OR=33, CI: 2.2-1405.6, p=0.03). Further adjustments found that obesity, sex (male), and elevated alkaline phosphatase level were independent risk factors for PEP (Table 1).
Discussion: This single-center cohort study revealed an increased risk of developing PEP in patients who underwent CCY with IOC, followed by ERCP.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Isabelle Nguyen indicated no relevant financial relationships.
David Leung indicated no relevant financial relationships.
Leah Puglisi indicated no relevant financial relationships.
Franklin Tsai indicated no relevant financial relationships.
Walter Coyle indicated no relevant financial relationships.
Isabelle Nguyen, MD1, David Leung, MD2, Leah Puglisi, MS3, Franklin Tsai, MD2, Walter Coyle, MD2. P0064 - Effect of Positive Intraoperative Cholangiogram on the Rates of Post Endoscopic Retrograde Cholangiopancreatography (ERCP) Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
