Sunday Poster Session
Category: Biliary/Pancreas
P0004 - Percutaneous Transhepatic Biliary Drainage versus Endoscopic Retrograde Cholangiopancreatography for Biliary Drainage in Liver Transplant Recipients
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Bhanu Siva Mohan Pinnam, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Bhanu Siva Mohan Pinnam, MD1, Pius E. Ojemolon, MD1, Dushyant S. Dahiya, MD2, Abdul Mohammed, MD3, Mihir P. Shah, MD4, Saurabh Chandan, MD5, Harishankar Gopakumar, MD6, Sanket Basida, MD7, Daksh Ahluwalia, MD1, Manesh Kumar Gangwani, MD8, Hemant Mutneja, MD1, Seema Gandhi, MD1, Mustafa Arain, MD3, Muhammad K. Hasan, MD3, Sumant Inamdar, MD8
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2The University of Kansas School of Medicine, Kansas City, KS; 3AdventHealth, Orlando, FL; 4John H. Stroger, Jr. Hospital of Cook County, Cook County, IL; 5CHI Health Creighton University Medical Center, Omaha, NE; 6University of Illinois College of Medicine, Bloomington, IL; 7University of Missouri School of Medicine, Columbia, MO; 8University of Arkansas for Medical Sciences, Little Rock, AR
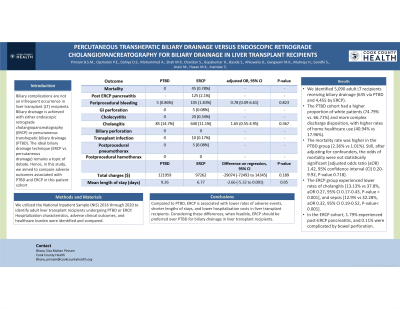
Introduction: Biliary complications are not an infrequent occurrence in liver transplant (LT) recipients. Biliary drainage is achieved with either endoscopic retrograde cholangiopancreatography (ERCP) or percutaneous transhepatic biliary drainage (PTBD). The ideal biliary drainage technique (ERCP vs. percutaneous drainage) remains a topic of debate. Hence, in this study, we aimed to compare adverse outcomes associated with PTBD and ERCP in this patient cohort.
Methods: We utilized the National Inpatient Sample (NIS) 2016 through 2020 to identify adult liver transplant recipients undergoing PTBD or ERCP. Hospitalization characteristics, adverse clinical outcomes, and healthcare burden were identified and compared.
Results: We identified 5,090 adult LT recipients receiving biliary drainage (635 via PTBD and 4,455 by ERCP). The PTBD cohort had a higher proportion of white patients (74.79% vs. 66.71%) and more complex discharge disposition, with higher rates of home healthcare use (40.94% vs 17.96%). The mortality rate was higher in the PTBD group (2.36% vs 1.01%). Still, after adjusting for confounders, the odds of mortality were not statistically significant [adjusted odds ratio (aOR) 1.42, 95% confidence interval (CI) 0.20-9.92, P-value 0.718]. The ERCP group experienced lower rates of cholangitis [13.13% vs 37.8%, aOR 0.27, 95% CI 0.17-0.43, P-value < 0.001], and sepsis [12.9% vs 32.28%, aOR 0.32, 95% CI 0.19-0.52, P-value< 0.001]. In the ERCP cohort, 1.79% experienced post-ERCP pancreatitis, and 0.11% were complicated by bowel perforation.
Discussion: Compared to PTBD, ERCP is associated with lower rates of adverse events, shorter lengths of stays, and lower hospitalization costs in liver transplant recipients. Considering these differences, when feasible, ERCP should be preferred over PTBD for biliary drainage in liver transplant recipients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Bhanu Siva Mohan Pinnam, MD1, Pius E. Ojemolon, MD1, Dushyant S. Dahiya, MD2, Abdul Mohammed, MD3, Mihir P. Shah, MD4, Saurabh Chandan, MD5, Harishankar Gopakumar, MD6, Sanket Basida, MD7, Daksh Ahluwalia, MD1, Manesh Kumar Gangwani, MD8, Hemant Mutneja, MD1, Seema Gandhi, MD1, Mustafa Arain, MD3, Muhammad K. Hasan, MD3, Sumant Inamdar, MD8. P0004 - Percutaneous Transhepatic Biliary Drainage versus Endoscopic Retrograde Cholangiopancreatography for Biliary Drainage in Liver Transplant Recipients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2The University of Kansas School of Medicine, Kansas City, KS; 3AdventHealth, Orlando, FL; 4John H. Stroger, Jr. Hospital of Cook County, Cook County, IL; 5CHI Health Creighton University Medical Center, Omaha, NE; 6University of Illinois College of Medicine, Bloomington, IL; 7University of Missouri School of Medicine, Columbia, MO; 8University of Arkansas for Medical Sciences, Little Rock, AR
Introduction: Biliary complications are not an infrequent occurrence in liver transplant (LT) recipients. Biliary drainage is achieved with either endoscopic retrograde cholangiopancreatography (ERCP) or percutaneous transhepatic biliary drainage (PTBD). The ideal biliary drainage technique (ERCP vs. percutaneous drainage) remains a topic of debate. Hence, in this study, we aimed to compare adverse outcomes associated with PTBD and ERCP in this patient cohort.
Methods: We utilized the National Inpatient Sample (NIS) 2016 through 2020 to identify adult liver transplant recipients undergoing PTBD or ERCP. Hospitalization characteristics, adverse clinical outcomes, and healthcare burden were identified and compared.
Results: We identified 5,090 adult LT recipients receiving biliary drainage (635 via PTBD and 4,455 by ERCP). The PTBD cohort had a higher proportion of white patients (74.79% vs. 66.71%) and more complex discharge disposition, with higher rates of home healthcare use (40.94% vs 17.96%). The mortality rate was higher in the PTBD group (2.36% vs 1.01%). Still, after adjusting for confounders, the odds of mortality were not statistically significant [adjusted odds ratio (aOR) 1.42, 95% confidence interval (CI) 0.20-9.92, P-value 0.718]. The ERCP group experienced lower rates of cholangitis [13.13% vs 37.8%, aOR 0.27, 95% CI 0.17-0.43, P-value < 0.001], and sepsis [12.9% vs 32.28%, aOR 0.32, 95% CI 0.19-0.52, P-value< 0.001]. In the ERCP cohort, 1.79% experienced post-ERCP pancreatitis, and 0.11% were complicated by bowel perforation.
Discussion: Compared to PTBD, ERCP is associated with lower rates of adverse events, shorter lengths of stays, and lower hospitalization costs in liver transplant recipients. Considering these differences, when feasible, ERCP should be preferred over PTBD for biliary drainage in liver transplant recipients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Bhanu Siva Mohan Pinnam indicated no relevant financial relationships.
Pius Ojemolon indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Abdul Mohammed indicated no relevant financial relationships.
Mihir Shah indicated no relevant financial relationships.
Saurabh Chandan indicated no relevant financial relationships.
Harishankar Gopakumar indicated no relevant financial relationships.
Sanket Basida indicated no relevant financial relationships.
Daksh Ahluwalia indicated no relevant financial relationships.
Manesh Kumar Gangwani indicated no relevant financial relationships.
Hemant Mutneja indicated no relevant financial relationships.
Seema Gandhi indicated no relevant financial relationships.
Mustafa Arain indicated no relevant financial relationships.
Muhammad Hasan: Boston Scientific – Consultant. microtech – Consultant. Neptune Medical – Consultant. Olympus – Consultant.
Sumant Inamdar indicated no relevant financial relationships.
Bhanu Siva Mohan Pinnam, MD1, Pius E. Ojemolon, MD1, Dushyant S. Dahiya, MD2, Abdul Mohammed, MD3, Mihir P. Shah, MD4, Saurabh Chandan, MD5, Harishankar Gopakumar, MD6, Sanket Basida, MD7, Daksh Ahluwalia, MD1, Manesh Kumar Gangwani, MD8, Hemant Mutneja, MD1, Seema Gandhi, MD1, Mustafa Arain, MD3, Muhammad K. Hasan, MD3, Sumant Inamdar, MD8. P0004 - Percutaneous Transhepatic Biliary Drainage versus Endoscopic Retrograde Cholangiopancreatography for Biliary Drainage in Liver Transplant Recipients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
