Sunday Poster Session
Category: Biliary/Pancreas
P0006 - Are Outcomes Truly Different in Patients with Acute Pancreatitis Across All Age?
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- DK
Donghyun Ko, MD
Yale-New Haven Health/Bridgeport Hospital
Bridgeport, CT
Presenting Author(s)
Donghyun Ko, MD1, Do Han Kim, MD2, Sharon Narvaez, MD3, Luis Nieto, MD4, Pedro Palacios-Argueta, MD5, Paul Kroner, MD, MSc6, Frank J. Lukens, MD7
1Yale-New Haven Health/Bridgeport Hospital, Bridgeport, CT; 2Mount Sinai Morningside and West, Icahn School of Medicine at Mount Sinai, New York, NY; 3Universidad de Guayaquil, School of Medicine, Atlanta, GA; 4Emory School of Medicine, Atlanta, GA; 5Mayo Clinic Florida, Jacksonville, FL; 6Riverside Regional Medical Center, Newport News, VA; 7Mayo Clinic, Jacksonville, FL
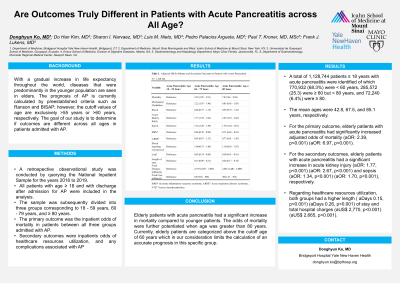
Introduction: With a gradual increase in life expectancy throughout the world, diseases that were predominantly in the younger population are seen in elders. The prognosis of AP is currently calculated by preestablished criteria such as Ranson and BISAP; however, the cutoff values of age are exclusively >55 years and >60 years, respectively. The goal of our study is to determine if outcomes are different across all ages in patients admitted with AP.
Methods: A retrospective observational study was conducted by querying the National Inpatient Sample for the years 2016 to 2019. All patients with age ≥ 18 and with discharge after admission for AP were included in the analysis. The sample was subsequently divided into three groups corresponding to 18 - 59 years, 60 - 79 years, and ≥ 80 years. The primary outcome was the inpatient odds of mortality in patients between all three groups admitted with AP. Secondary outcomes were inpatients odds of healthcare resources utilization and any complications associated with AP. Multivariate regression analyses were used to adjust for gender, insurance status, Charlson Comorbidity Index, income, hospital region, location, size, teaching status, comorbidities, and inpatients complications.
Results: A total of 1,128,744 patients ≥ 18 years with acute pancreatitis were identified of which 770,932 (68.3%) were < 60 years, 285,572 (25.3) were ≥ 60 but < 80 years, and 72,240 (6.4%) were ≥ 80. The mean ages were 42.8, 67.5, and 85.1 years respectively. For the primary outcome, elderly patients with acute pancreatitis had significantly increased adjusted odds of mortality (aOR: 2.39, p< 0.001) (aOR: 6.97, p< 0.001). For the secondary outcomes, elderly patients with acute pancreatitis had a significant increase in acute kidney injury (aOR: 1.77, p< 0.001) (aOR: 2.67, p< 0.001), and sepsis (aOR: 1.34, p< 0.001) (aOR: 1.70, p< 0.001). Regarding healthcare resources utilization, both groups had a higher length ( aDays 0.15, p< 0.001) (aDays 0.26, p< 0.001) of stay and total hospital charges (aUS$ 2,770, p< 0.001) (aUS$ 2,665, p< 0.001).
Discussion: Elderly patients with acute pancreatitis had a significant increase in mortality compared to younger patients. The odds of mortality were further potentiated when age was greater than 80 years. Currently, elderly patients are categorized above the cutoff age of 60 years which in our consideration limits the calculate an accurate prognosis.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Donghyun Ko, MD1, Do Han Kim, MD2, Sharon Narvaez, MD3, Luis Nieto, MD4, Pedro Palacios-Argueta, MD5, Paul Kroner, MD, MSc6, Frank J. Lukens, MD7. P0006 - Are Outcomes Truly Different in Patients with Acute Pancreatitis Across All Age?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Yale-New Haven Health/Bridgeport Hospital, Bridgeport, CT; 2Mount Sinai Morningside and West, Icahn School of Medicine at Mount Sinai, New York, NY; 3Universidad de Guayaquil, School of Medicine, Atlanta, GA; 4Emory School of Medicine, Atlanta, GA; 5Mayo Clinic Florida, Jacksonville, FL; 6Riverside Regional Medical Center, Newport News, VA; 7Mayo Clinic, Jacksonville, FL
Introduction: With a gradual increase in life expectancy throughout the world, diseases that were predominantly in the younger population are seen in elders. The prognosis of AP is currently calculated by preestablished criteria such as Ranson and BISAP; however, the cutoff values of age are exclusively >55 years and >60 years, respectively. The goal of our study is to determine if outcomes are different across all ages in patients admitted with AP.
Methods: A retrospective observational study was conducted by querying the National Inpatient Sample for the years 2016 to 2019. All patients with age ≥ 18 and with discharge after admission for AP were included in the analysis. The sample was subsequently divided into three groups corresponding to 18 - 59 years, 60 - 79 years, and ≥ 80 years. The primary outcome was the inpatient odds of mortality in patients between all three groups admitted with AP. Secondary outcomes were inpatients odds of healthcare resources utilization and any complications associated with AP. Multivariate regression analyses were used to adjust for gender, insurance status, Charlson Comorbidity Index, income, hospital region, location, size, teaching status, comorbidities, and inpatients complications.
Results: A total of 1,128,744 patients ≥ 18 years with acute pancreatitis were identified of which 770,932 (68.3%) were < 60 years, 285,572 (25.3) were ≥ 60 but < 80 years, and 72,240 (6.4%) were ≥ 80. The mean ages were 42.8, 67.5, and 85.1 years respectively. For the primary outcome, elderly patients with acute pancreatitis had significantly increased adjusted odds of mortality (aOR: 2.39, p< 0.001) (aOR: 6.97, p< 0.001). For the secondary outcomes, elderly patients with acute pancreatitis had a significant increase in acute kidney injury (aOR: 1.77, p< 0.001) (aOR: 2.67, p< 0.001), and sepsis (aOR: 1.34, p< 0.001) (aOR: 1.70, p< 0.001). Regarding healthcare resources utilization, both groups had a higher length ( aDays 0.15, p< 0.001) (aDays 0.26, p< 0.001) of stay and total hospital charges (aUS$ 2,770, p< 0.001) (aUS$ 2,665, p< 0.001).
Discussion: Elderly patients with acute pancreatitis had a significant increase in mortality compared to younger patients. The odds of mortality were further potentiated when age was greater than 80 years. Currently, elderly patients are categorized above the cutoff age of 60 years which in our consideration limits the calculate an accurate prognosis.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Donghyun Ko indicated no relevant financial relationships.
Do Han Kim indicated no relevant financial relationships.
Sharon Narvaez indicated no relevant financial relationships.
Luis Nieto indicated no relevant financial relationships.
Pedro Palacios-Argueta indicated no relevant financial relationships.
Paul Kroner indicated no relevant financial relationships.
Frank J. Lukens indicated no relevant financial relationships.
Donghyun Ko, MD1, Do Han Kim, MD2, Sharon Narvaez, MD3, Luis Nieto, MD4, Pedro Palacios-Argueta, MD5, Paul Kroner, MD, MSc6, Frank J. Lukens, MD7. P0006 - Are Outcomes Truly Different in Patients with Acute Pancreatitis Across All Age?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
