Sunday Poster Session
Category: Biliary/Pancreas
P0007 - Endoscopic vs Surgical Management of Pancreatic Necrosis: A Systematic Review and Meta-Analysis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Sree Maneesha Sunkara, MBBS, MPH.
Malla Reddy Institute of Medical Sciences, MA
Presenting Author(s)
Sree Maneesha Sunkara, MBBS, MPH.1, Mahek Fatima, MBBS2, Archana Priyadarsini, MBBS3, Ashwith Reddy Gaddam, MD4, Sreeja Cherukuru, MBBS5, Binay K. Panjiyar, MBBS6
1Malla Reddy Institute of Medical Sciences, Ashland, MA; 2Osmania General Hospital and Medical College, Hyderabad, Telangana, India; 3Dr Somervell Memorial CSI Medical College, Missouri City, TX; 4University of Kansas Medical Center, Kamareddy, Telangana, India; 5Sri Venkateswara Medical College, Tirupati, Andhra Pradesh, India; 6Harvard Medical School, Boston, MA
Introduction: Necrotizing pancreatitis is a complication of acute pancreatitis that develops in 10-20% of cases. The optimal treatment of interventional procedures remains a topic for discussion, primarily due to the condition's heterogeneity. We conducted a systematic review and meta-analysis to compare endoscopic and surgical necrosectomy's primary and secondary outcomes.
Methods: We conducted a comprehensive literature search using databases including PubMed, Google Scholar, BioMed Central, ScienceDirect, Cochrane Library, and ClinicalTrials.gov, from 2010 to 2024. Five randomized controlled trials (RCTs) and three observational studies with a total of 525 patients, with 275 undergoing endoscopic and 250 undergoing surgical procedures were included in the study. The primary outcome of interest is mortality, and secondary outcomes including multiple organ failure, incisional hernia, fistula formation, endocrine and exocrine insufficiency, and intrabdominal bleeding were compared. Statistical analysis was performed using Review Manager (RevMan) 5.4.1 and the Random-effect model.
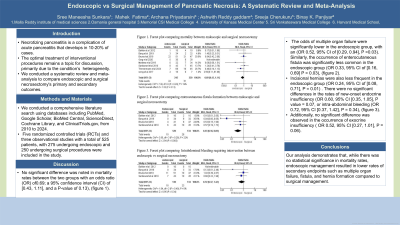
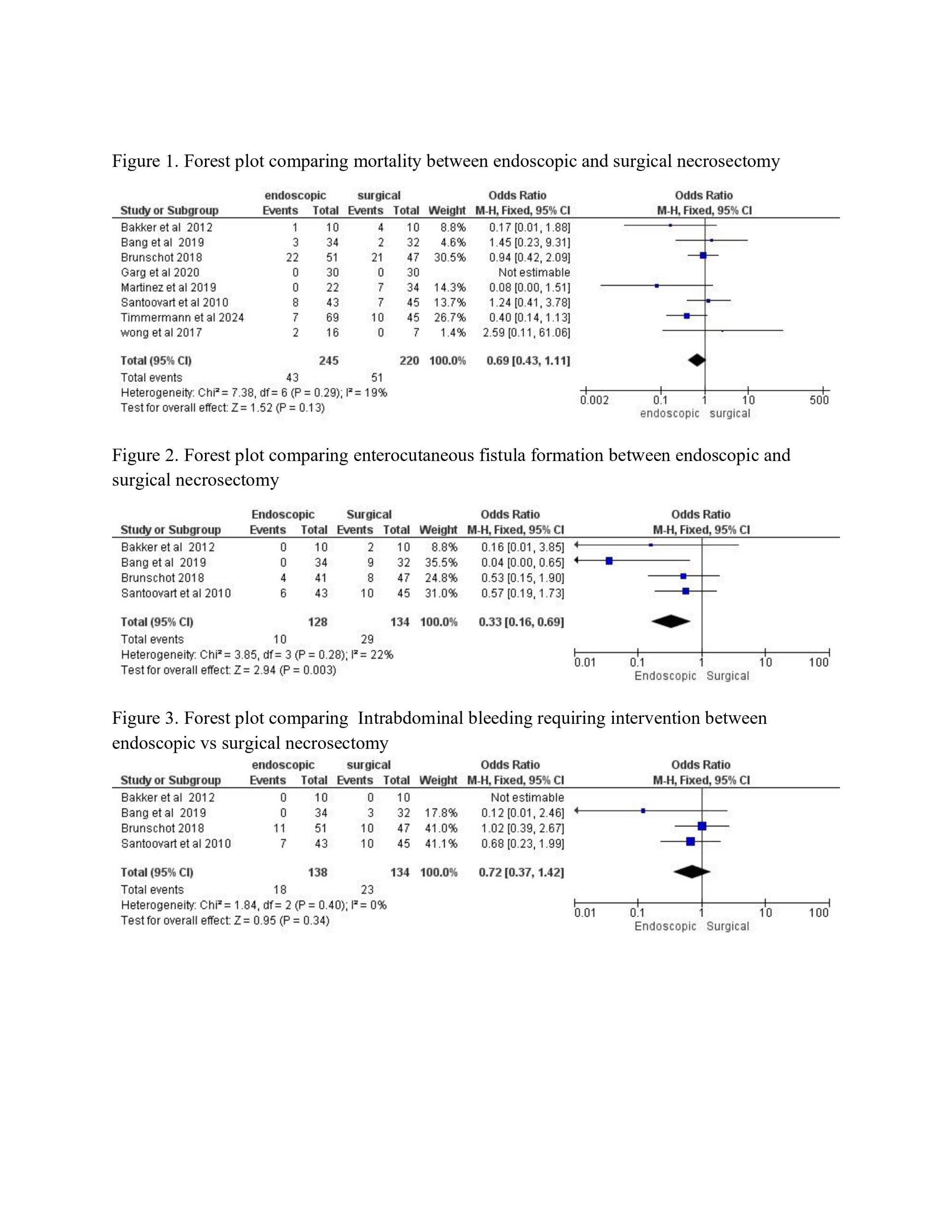
Results: No significant difference was noted in mortality rates between the two groups with an odds ratio (OR) of 0.69; a 95% confidence interval (CI) of [0.43, 1.11], and a P-value of 0.13), (figure 1). The odds of multiple organ failure were significantly lower in the endoscopic group, with an (OR 0.52, 95% CI of [0.29, 0.94], P = 0.03). Similarly, the occurrence of enterocutaneous fistula was significantly less common in the endoscopic group (OR 0.33, 95% CI of [0.16, 0.69] P = 0.03), (figure 2). Incisional hernias were also less frequent in the endoscopic group (OR 0.24, 95% CI of [0.08, 0.71], P = 0.01) . There were no significant differences in the rates of new-onset endocrine insufficiency (OR 0.60, 95% CI [0.35, 1.05], P value = 0.07, or intra-abdominal bleeding (OR 0.72, 95% CI [0.37, 1.42], P = 0.34), (figure 3). Additionally, no significant difference was observed in the occurrence of exocrine insufficiency ( OR 0.52, 95% CI [0.27, 1.01], P = 0.06).
Discussion: Our analysis demonstrates that, while there was no statistical significance in mortality rates, endoscopic management resulted in lower rates of secondary endpoints such as multiple organ failure, fistula, and hernia formation compared to surgical management.
Disclosures:
Sree Maneesha Sunkara, MBBS, MPH.1, Mahek Fatima, MBBS2, Archana Priyadarsini, MBBS3, Ashwith Reddy Gaddam, MD4, Sreeja Cherukuru, MBBS5, Binay K. Panjiyar, MBBS6. P0007 - Endoscopic vs Surgical Management of Pancreatic Necrosis: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Malla Reddy Institute of Medical Sciences, Ashland, MA; 2Osmania General Hospital and Medical College, Hyderabad, Telangana, India; 3Dr Somervell Memorial CSI Medical College, Missouri City, TX; 4University of Kansas Medical Center, Kamareddy, Telangana, India; 5Sri Venkateswara Medical College, Tirupati, Andhra Pradesh, India; 6Harvard Medical School, Boston, MA
Introduction: Necrotizing pancreatitis is a complication of acute pancreatitis that develops in 10-20% of cases. The optimal treatment of interventional procedures remains a topic for discussion, primarily due to the condition's heterogeneity. We conducted a systematic review and meta-analysis to compare endoscopic and surgical necrosectomy's primary and secondary outcomes.
Methods: We conducted a comprehensive literature search using databases including PubMed, Google Scholar, BioMed Central, ScienceDirect, Cochrane Library, and ClinicalTrials.gov, from 2010 to 2024. Five randomized controlled trials (RCTs) and three observational studies with a total of 525 patients, with 275 undergoing endoscopic and 250 undergoing surgical procedures were included in the study. The primary outcome of interest is mortality, and secondary outcomes including multiple organ failure, incisional hernia, fistula formation, endocrine and exocrine insufficiency, and intrabdominal bleeding were compared. Statistical analysis was performed using Review Manager (RevMan) 5.4.1 and the Random-effect model.
Results: No significant difference was noted in mortality rates between the two groups with an odds ratio (OR) of 0.69; a 95% confidence interval (CI) of [0.43, 1.11], and a P-value of 0.13), (figure 1). The odds of multiple organ failure were significantly lower in the endoscopic group, with an (OR 0.52, 95% CI of [0.29, 0.94], P = 0.03). Similarly, the occurrence of enterocutaneous fistula was significantly less common in the endoscopic group (OR 0.33, 95% CI of [0.16, 0.69] P = 0.03), (figure 2). Incisional hernias were also less frequent in the endoscopic group (OR 0.24, 95% CI of [0.08, 0.71], P = 0.01) . There were no significant differences in the rates of new-onset endocrine insufficiency (OR 0.60, 95% CI [0.35, 1.05], P value = 0.07, or intra-abdominal bleeding (OR 0.72, 95% CI [0.37, 1.42], P = 0.34), (figure 3). Additionally, no significant difference was observed in the occurrence of exocrine insufficiency ( OR 0.52, 95% CI [0.27, 1.01], P = 0.06).
Discussion: Our analysis demonstrates that, while there was no statistical significance in mortality rates, endoscopic management resulted in lower rates of secondary endpoints such as multiple organ failure, fistula, and hernia formation compared to surgical management.
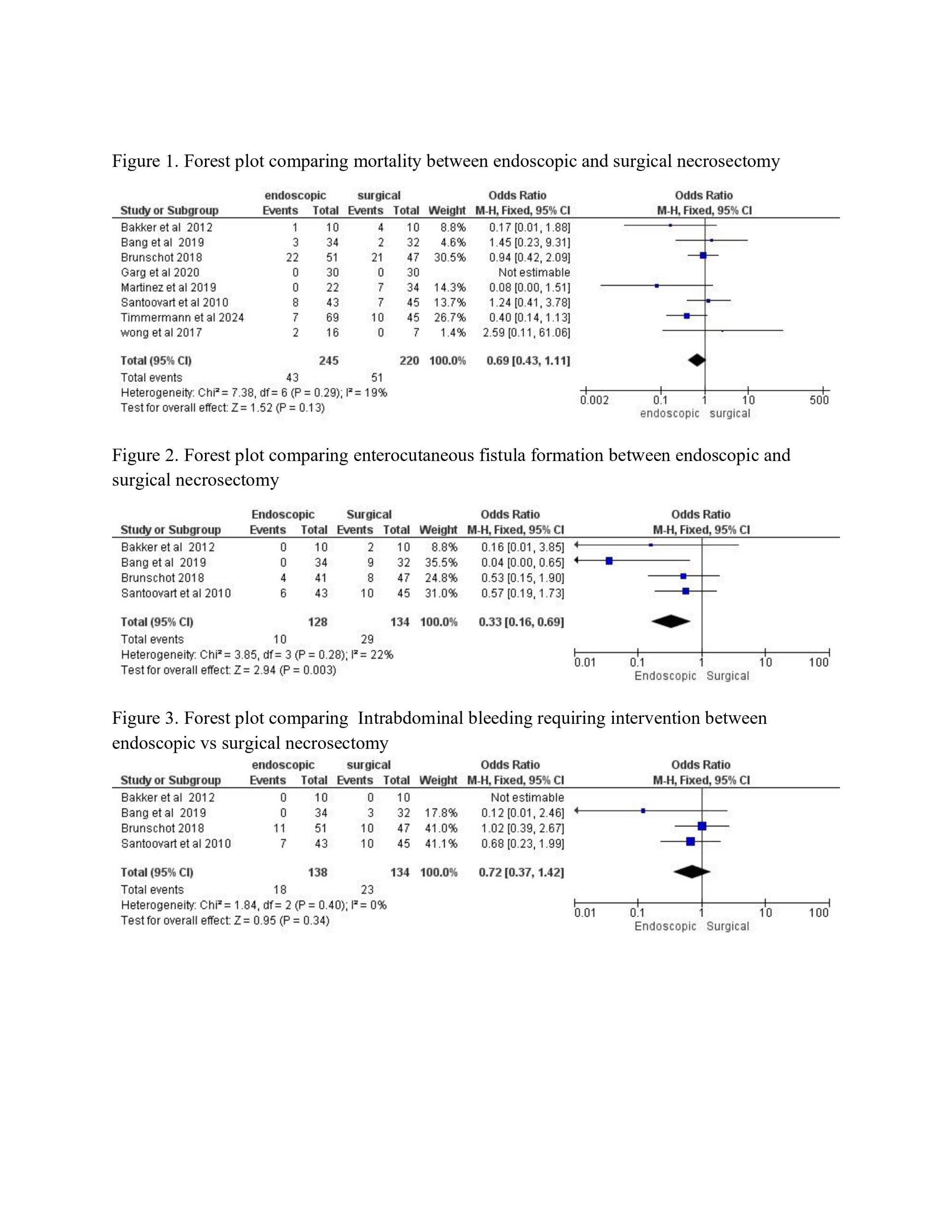
Figure: Forest Plots comparing primary and secondary outcomes between endoscopic and surgical management.
Disclosures:
Sree Maneesha Sunkara indicated no relevant financial relationships.
Mahek Fatima indicated no relevant financial relationships.
Archana Priyadarsini indicated no relevant financial relationships.
Ashwith Reddy Gaddam indicated no relevant financial relationships.
Sreeja Cherukuru indicated no relevant financial relationships.
Binay Panjiyar indicated no relevant financial relationships.
Sree Maneesha Sunkara, MBBS, MPH.1, Mahek Fatima, MBBS2, Archana Priyadarsini, MBBS3, Ashwith Reddy Gaddam, MD4, Sreeja Cherukuru, MBBS5, Binay K. Panjiyar, MBBS6. P0007 - Endoscopic vs Surgical Management of Pancreatic Necrosis: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
