Sunday Poster Session
Category: Biliary/Pancreas
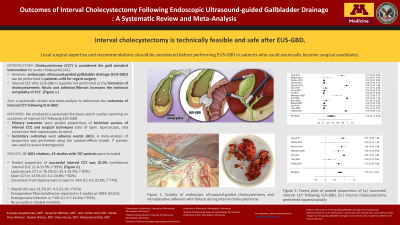
P0008 - Outcomes of Interval Cholecystectomy Following Endoscopic Ultrasound-Guided Gallbladder Drainage: A Systematic Review and Meta-Analysis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Suchapa Arayakarnkul, MD
University of Minnesota
Minneapolis, MN
Presenting Author(s)
Suchapa Arayakarnkul, MD1, Jacquelin Blomker, MD1, Amir Sultan Seid, MD1, Nicole Theis-Mahon, 1, Natalie Wilson, MD1, Rahul Karna, MD2, Mohammad Bilal, MD3
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN; 3University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Cholecystectomy is the gold standard for management of acute cholecystitis (AC). However, AC patients who are medically unfit for surgery at index presentation can undergo endoscopic ultrasound-guided gallbladder drainage (EUS-GBD) for treatment of AC. EUS-GBD is typically limited to patients who will not be candidates for interval cholecystectomy as the formation of cholecystoenteric fistula can make future surgery challenging. Recent studies have suggested feasibility of EUS-GB as a bridge to subsequent surgery. We aim to conduct a systematic review and meta-analysis to determine the outcomes of interval cholecystectomy in patients with previous EUS-GBD.
Methods: We conducted a literature search of multiple electronic databases (inception-June 2024) for studies evaluating outcomes of interval cholecystectomy following EUS-GBD. Primary outcomes were pooled proportion of patients undergoing cholecystectomy, conversion rate of laparoscopic-to-open cholecystectomy, rates of open cholecystectomy and rate of adverse events (AEs). Secondary outcomes were procedural time, length of stay (LOS), and mortality. A meta-analysis of proportion was performed using the random-effects model. I² statistic was used to assess heterogeneity.
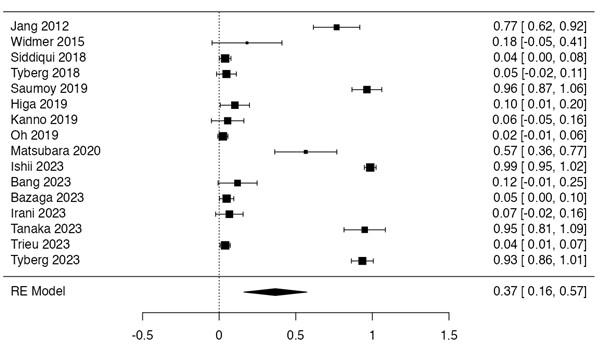
Results: Out of 1001 citations, 16 studies including 716 patients (51.8% male, mean age 71.7±14.8, mean Charlson Comorbidity Index 5.93±3.5) who had previously undergone EUS-GBD [stent site: duodenum 47.5%; stomach 27.7%; jejunum 0.7%] were analyzed. (Table 1) Pooled proportion of successful interval cholecystectomy was 0.37 (CI: 0.16-0.57; I2 99%) (Figure 1) [laparoscopic: 0.74 (CI: 0.6-0.88; I2 82%); open: 0.13 (CI: 0.04-0.22; I2 80%); laparoscopic converted to open: 0.16 (CI: 0.06-0.26; I2 77%)]. None of the studies reported aborted surgery. Interval cholecystectomy was performed after 52.8±65.5 days from the initial EUS-GBD. Pooled proportion of overall AEs was 0.16 (CI: 0.06-0.25; I2 65%), including postoperative infection: 0.1 (CI: 0.02-0.18; I2 70%). Mean procedural time was 120±67.3 minutes, with mean LOS 5.8±3.6 days. There was no procedure-related mortality.
Discussion: Our study demonstrates that interval cholecystectomy is technically safe and feasible after EUS-GBD. Nearly 75% of patients underwent successful laparoscopic cholecystectomy, with conversion to open reported in only 16%. However, these results could have a selection bias due to candidate selection for interval cholecystectomy after EUS-GBD.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Suchapa Arayakarnkul, MD1, Jacquelin Blomker, MD1, Amir Sultan Seid, MD1, Nicole Theis-Mahon, 1, Natalie Wilson, MD1, Rahul Karna, MD2, Mohammad Bilal, MD3. P0008 - Outcomes of Interval Cholecystectomy Following Endoscopic Ultrasound-Guided Gallbladder Drainage: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN; 3University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Cholecystectomy is the gold standard for management of acute cholecystitis (AC). However, AC patients who are medically unfit for surgery at index presentation can undergo endoscopic ultrasound-guided gallbladder drainage (EUS-GBD) for treatment of AC. EUS-GBD is typically limited to patients who will not be candidates for interval cholecystectomy as the formation of cholecystoenteric fistula can make future surgery challenging. Recent studies have suggested feasibility of EUS-GB as a bridge to subsequent surgery. We aim to conduct a systematic review and meta-analysis to determine the outcomes of interval cholecystectomy in patients with previous EUS-GBD.
Methods: We conducted a literature search of multiple electronic databases (inception-June 2024) for studies evaluating outcomes of interval cholecystectomy following EUS-GBD. Primary outcomes were pooled proportion of patients undergoing cholecystectomy, conversion rate of laparoscopic-to-open cholecystectomy, rates of open cholecystectomy and rate of adverse events (AEs). Secondary outcomes were procedural time, length of stay (LOS), and mortality. A meta-analysis of proportion was performed using the random-effects model. I² statistic was used to assess heterogeneity.
Results: Out of 1001 citations, 16 studies including 716 patients (51.8% male, mean age 71.7±14.8, mean Charlson Comorbidity Index 5.93±3.5) who had previously undergone EUS-GBD [stent site: duodenum 47.5%; stomach 27.7%; jejunum 0.7%] were analyzed. (Table 1) Pooled proportion of successful interval cholecystectomy was 0.37 (CI: 0.16-0.57; I2 99%) (Figure 1) [laparoscopic: 0.74 (CI: 0.6-0.88; I2 82%); open: 0.13 (CI: 0.04-0.22; I2 80%); laparoscopic converted to open: 0.16 (CI: 0.06-0.26; I2 77%)]. None of the studies reported aborted surgery. Interval cholecystectomy was performed after 52.8±65.5 days from the initial EUS-GBD. Pooled proportion of overall AEs was 0.16 (CI: 0.06-0.25; I2 65%), including postoperative infection: 0.1 (CI: 0.02-0.18; I2 70%). Mean procedural time was 120±67.3 minutes, with mean LOS 5.8±3.6 days. There was no procedure-related mortality.
Discussion: Our study demonstrates that interval cholecystectomy is technically safe and feasible after EUS-GBD. Nearly 75% of patients underwent successful laparoscopic cholecystectomy, with conversion to open reported in only 16%. However, these results could have a selection bias due to candidate selection for interval cholecystectomy after EUS-GBD.
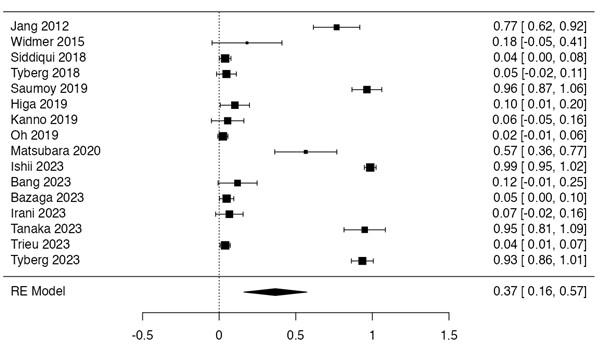
Figure: Figure 1. Forest plot for pooled proportion of interval cholecystectomy following endoscopic ultrasound-guided gallbladder drainage
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Suchapa Arayakarnkul indicated no relevant financial relationships.
Jacquelin Blomker indicated no relevant financial relationships.
Amir Sultan Seid indicated no relevant financial relationships.
Nicole Theis-Mahon indicated no relevant financial relationships.
Natalie Wilson indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Speakers Bureau.
Suchapa Arayakarnkul, MD1, Jacquelin Blomker, MD1, Amir Sultan Seid, MD1, Nicole Theis-Mahon, 1, Natalie Wilson, MD1, Rahul Karna, MD2, Mohammad Bilal, MD3. P0008 - Outcomes of Interval Cholecystectomy Following Endoscopic Ultrasound-Guided Gallbladder Drainage: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
