Tuesday Poster Session
Category: Esophagus
P3969 - A Case of Benign Spontaneous Pneumomediastinum
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Yende Grell, MD
New York-Presbyterian / Weill Cornell Medical Center
New York, NY
Presenting Author(s)
Yende Grell, MD1, Emily Smith, MD2, David Wan, MD1
1New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 2New York-Presbyterian/Weill Cornell, New York, NY
Introduction: Pneumomediastinum, in the absence of iatrogenic or traumatic etiologies, underlying lung disease, or obvious inciting events, is classified as benign spontaneous pneumomediastinum (SPM). We present the case of a woman with pneumomediastinum without evidence of esophageal injury, trauma, or recent proceduralization who was treated conservatively and discharged without intervention.
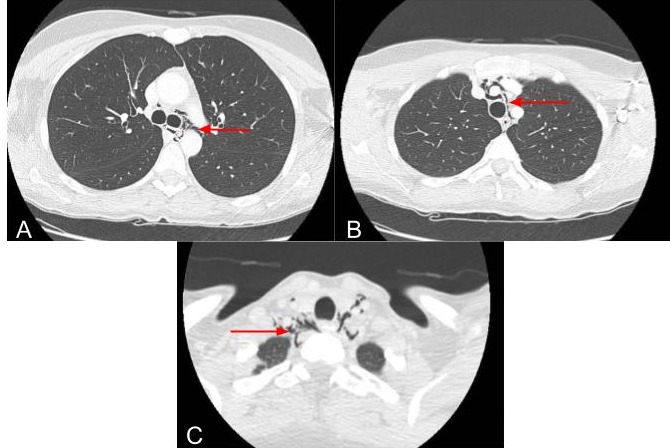
Case Description/Methods: A 40-year-old woman with no significant medical history presented with upper chest pain for 3 hours. The patient reported a history of subacute recurrent emesis since starting semaglutide 6 months prior. She vaped socially and denied any other drug use. On the day of presentation, she experienced acute 10/10 upper chest pain that radiated to her back and neck after eating a meal. Her vital signs were normal, and her labs were unremarkable. Physical exam was without chest wall crepitus. Computed tomography scan of the chest and neck with intravenous and oral contrast showed pneumomediastinum tracking along the left mainstem bronchus and upper trachea into the neck without contrast extravasation or esophageal obstruction and with passage of contrast to the gastroesophageal junction (Figure 1). Gastroenterology and thoracic surgery were consulted. Given her hemodynamic stability, no signs of sepsis, and lack of impaction, the patient was treated conservatively with a proton pump inhibitor, antibiotics, antiemetics, and NPO diet. Antibiotics were discontinued after cultures were negative, her pain resolved, and she was able to tolerate a regular diet by time of discharge one day later.
Discussion: SPM is thought to occur as a result of a sudden increase in intrathoracic pressure which increases intra-alveolar pressure and leads to rupture. This is typically precipitated by activities triggering a valsalva maneuver such as vomiting in this case. There is also increasing literature on vaping-induced SPM, though this has been associated with daily use which was not the case for this patient who endorsed intermittent social use.
SPM responds well to conservative treatment, and small retrospective studies have shown similar outcomes for patients with SPM who were hospitalized compared to those treated in the ambulatory setting. This case of a young woman with SPM who was hospitalized for one day and discharged without need for additional procedures or antibiotics highlights novel risk factors that should be considered for SPM and the need for larger, prospective studies on ambulatory treatment.
Disclosures:
Yende Grell, MD1, Emily Smith, MD2, David Wan, MD1. P3969 - A Case of Benign Spontaneous Pneumomediastinum, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 2New York-Presbyterian/Weill Cornell, New York, NY
Introduction: Pneumomediastinum, in the absence of iatrogenic or traumatic etiologies, underlying lung disease, or obvious inciting events, is classified as benign spontaneous pneumomediastinum (SPM). We present the case of a woman with pneumomediastinum without evidence of esophageal injury, trauma, or recent proceduralization who was treated conservatively and discharged without intervention.
Case Description/Methods: A 40-year-old woman with no significant medical history presented with upper chest pain for 3 hours. The patient reported a history of subacute recurrent emesis since starting semaglutide 6 months prior. She vaped socially and denied any other drug use. On the day of presentation, she experienced acute 10/10 upper chest pain that radiated to her back and neck after eating a meal. Her vital signs were normal, and her labs were unremarkable. Physical exam was without chest wall crepitus. Computed tomography scan of the chest and neck with intravenous and oral contrast showed pneumomediastinum tracking along the left mainstem bronchus and upper trachea into the neck without contrast extravasation or esophageal obstruction and with passage of contrast to the gastroesophageal junction (Figure 1). Gastroenterology and thoracic surgery were consulted. Given her hemodynamic stability, no signs of sepsis, and lack of impaction, the patient was treated conservatively with a proton pump inhibitor, antibiotics, antiemetics, and NPO diet. Antibiotics were discontinued after cultures were negative, her pain resolved, and she was able to tolerate a regular diet by time of discharge one day later.
Discussion: SPM is thought to occur as a result of a sudden increase in intrathoracic pressure which increases intra-alveolar pressure and leads to rupture. This is typically precipitated by activities triggering a valsalva maneuver such as vomiting in this case. There is also increasing literature on vaping-induced SPM, though this has been associated with daily use which was not the case for this patient who endorsed intermittent social use.
SPM responds well to conservative treatment, and small retrospective studies have shown similar outcomes for patients with SPM who were hospitalized compared to those treated in the ambulatory setting. This case of a young woman with SPM who was hospitalized for one day and discharged without need for additional procedures or antibiotics highlights novel risk factors that should be considered for SPM and the need for larger, prospective studies on ambulatory treatment.
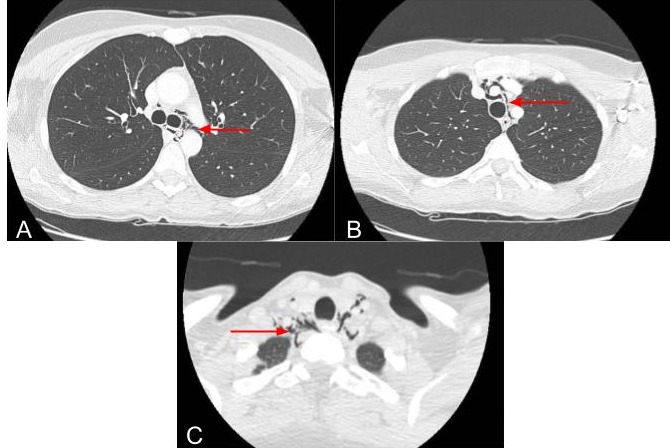
Figure: Figure 1. A. Free air along the left mainstem bronchus B. Free air along the trachea C. Free air along the upper trachea extending into the neck soft tissues.
Disclosures:
Yende Grell indicated no relevant financial relationships.
Emily Smith indicated no relevant financial relationships.
David Wan indicated no relevant financial relationships.
Yende Grell, MD1, Emily Smith, MD2, David Wan, MD1. P3969 - A Case of Benign Spontaneous Pneumomediastinum, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
