Tuesday Poster Session
Category: Esophagus
P4001 - More Than GERD: Unusual Histologic Findings of Lichenoid Esophagitis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Gabriel Sperling, MD
University of North Carolina Hospitals
Chapel Hill, NC
Presenting Author(s)
Gabriel Sperling, MD1, Eric Margulies, MD2, Richard Warneke, MD2
1University of North Carolina Hospitals, Chapel Hill, NC; 2University of Texas Medical Branch, Galveston, TX
Introduction: Lichenoid esophagitis (LE) describes a histologic pattern of injury that may be due to a variety of etiologies including lichen planus, infections, drugs, pill esophagitis, Crohn’s disease, and rheumatologic disorders. We present a rare case of LE presenting as GERD refractory to proton pump inhibitor (PPI) therapy in a patient without any risk factors associated with LE.
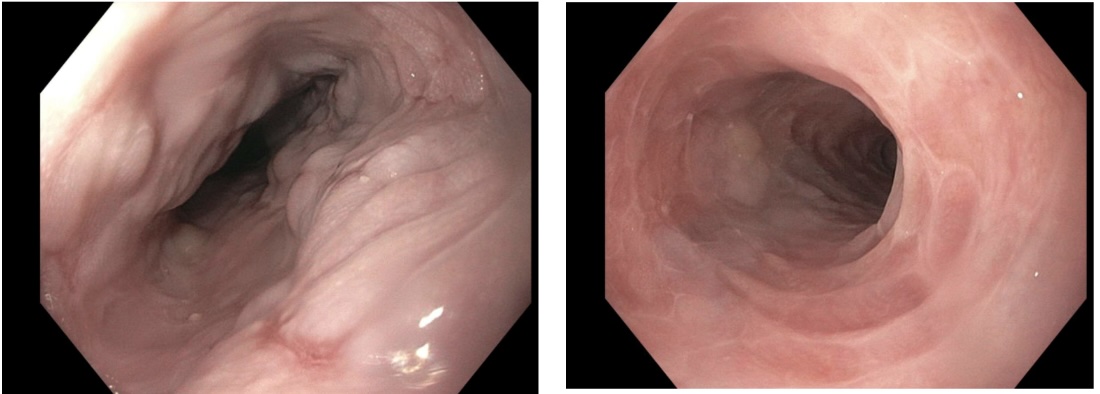
Case Description/Methods: A 58-year-old female with a history of atrial fibrillation, chronic venous thromboembolism, and obesity presented for evaluation of intermittent, sharp mid-epigastric pain, nausea, post-prandial retrosternal burning, and intermittent dysphagia. She was started on omeprazole 40mg daily for suspected GERD management, and an EGD was recommended but not completed due to financial concerns. She returned to clinic 10 months later with worsening symptoms despite appropriate PPI use, and now also having intermittent emesis. An EGD demonstrated diffuse congestion and erythema throughout the esophagus. Biopsies noted squamous mucosa with a lichenoid esophagitis pattern of injury in the upper and lower third of the esophagus. She tested negative for fungal infections and herpes virus, common infectious culprits. She was advised to continue the current omeprazole regimen while adding fluticasone 220mcg inhaler twice daily and close outpatient follow up.
Discussion: LE is a rare but well-recognized, nonspecific pattern of esophageal injury found more frequently in middle-age women. Histologic findings in LE typically demonstrate a prominent band-like lymphocytic infiltrate with intraepithelial lymphocytes and apoptotic keratinocytes (Civatte bodies). LE is an appropriate diagnostic term when clinical, histologic, and lab findings cannot specifically categorize the lichenoid inflammation, as seen in this patient. However, polypharmacy (defined as >3 medications at one time) may be contributing to the pattern of inflammation in this patient. Treatment typically relies on addressing the underlying etiology of LE. Management in this patient with unknown etiology was similar to those with esophageal lichen planus given the clinicopathologic overlap, including optimization of PPI therapy and the addition of topical or swallowed steroids. Frequent surveillance is necessary in patients with LE to prevent complications including esophageal strictures and to monitor for malignant transformation. We present this case to raise awareness of a rare, significant pathological entity without established management guidelines.
Disclosures:
Gabriel Sperling, MD1, Eric Margulies, MD2, Richard Warneke, MD2. P4001 - More Than GERD: Unusual Histologic Findings of Lichenoid Esophagitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of North Carolina Hospitals, Chapel Hill, NC; 2University of Texas Medical Branch, Galveston, TX
Introduction: Lichenoid esophagitis (LE) describes a histologic pattern of injury that may be due to a variety of etiologies including lichen planus, infections, drugs, pill esophagitis, Crohn’s disease, and rheumatologic disorders. We present a rare case of LE presenting as GERD refractory to proton pump inhibitor (PPI) therapy in a patient without any risk factors associated with LE.
Case Description/Methods: A 58-year-old female with a history of atrial fibrillation, chronic venous thromboembolism, and obesity presented for evaluation of intermittent, sharp mid-epigastric pain, nausea, post-prandial retrosternal burning, and intermittent dysphagia. She was started on omeprazole 40mg daily for suspected GERD management, and an EGD was recommended but not completed due to financial concerns. She returned to clinic 10 months later with worsening symptoms despite appropriate PPI use, and now also having intermittent emesis. An EGD demonstrated diffuse congestion and erythema throughout the esophagus. Biopsies noted squamous mucosa with a lichenoid esophagitis pattern of injury in the upper and lower third of the esophagus. She tested negative for fungal infections and herpes virus, common infectious culprits. She was advised to continue the current omeprazole regimen while adding fluticasone 220mcg inhaler twice daily and close outpatient follow up.
Discussion: LE is a rare but well-recognized, nonspecific pattern of esophageal injury found more frequently in middle-age women. Histologic findings in LE typically demonstrate a prominent band-like lymphocytic infiltrate with intraepithelial lymphocytes and apoptotic keratinocytes (Civatte bodies). LE is an appropriate diagnostic term when clinical, histologic, and lab findings cannot specifically categorize the lichenoid inflammation, as seen in this patient. However, polypharmacy (defined as >3 medications at one time) may be contributing to the pattern of inflammation in this patient. Treatment typically relies on addressing the underlying etiology of LE. Management in this patient with unknown etiology was similar to those with esophageal lichen planus given the clinicopathologic overlap, including optimization of PPI therapy and the addition of topical or swallowed steroids. Frequent surveillance is necessary in patients with LE to prevent complications including esophageal strictures and to monitor for malignant transformation. We present this case to raise awareness of a rare, significant pathological entity without established management guidelines.
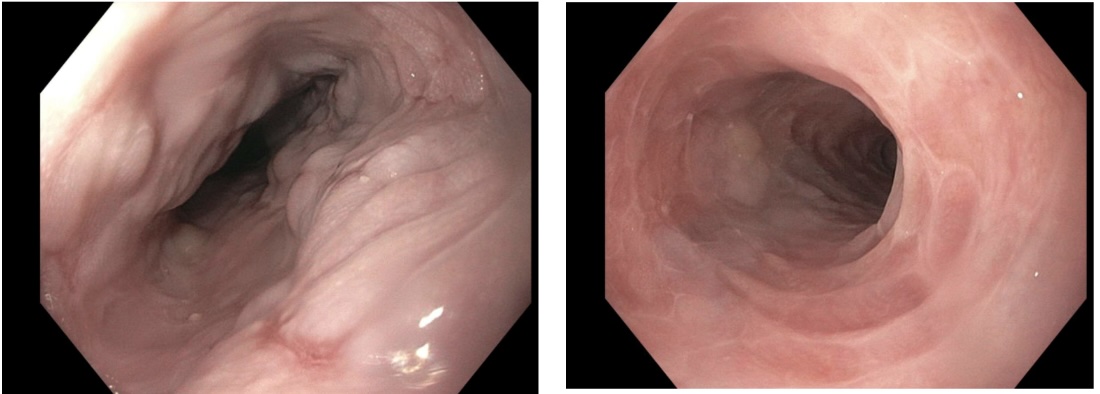
Figure: Figure 1. Congestion and erythema throughout the esophagus
Disclosures:
Gabriel Sperling indicated no relevant financial relationships.
Eric Margulies indicated no relevant financial relationships.
Richard Warneke indicated no relevant financial relationships.
Gabriel Sperling, MD1, Eric Margulies, MD2, Richard Warneke, MD2. P4001 - More Than GERD: Unusual Histologic Findings of Lichenoid Esophagitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
