Tuesday Poster Session
Category: Esophagus
P4004 - An Obscure Case of Dysphagia
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- YY
Yuhong Yang, MD
Mount Sinai Beth Israel, Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Yuhong Yang, MD1, Michael S.. Smith, MD, MBA2, Kimberly Cavaliere, MD3
1Mount Sinai Beth Israel, Icahn School of Medicine at Mount Sinai, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY; 3Icahn School of Medicine at Mount Sinai Morningside/West, New York, NY
Introduction: Ectopic gastric mucosa may appear anywhere in the gastrointestinal tract. Its most common location is the proximal esophagus, where it is also known as cervical inlet patches (CIP), and most often asymptomatic. However, when parietal cells are present, acid secretion can lead to symptoms and tissue damage. We present a patient with a large area of ectopic gastric mucosa complicated by peptic stricture.
Case Description/Methods: 53-year-old woman presented with ten years of dysphagia. She noted intermittent solid food dysphagia which progressively worsened. She reported a sensation of food remaining in her throat about twice a month, associated with chest pain and difficulty swallowing both water and saliva. Prior evaluation included a normal barium esophagram, upper endoscopy (EGD), and laryngoscopy. Empiric proton pump inhibitor (PPI) and intermittent fasting improved her dysphagia. A subsequent modified barium swallow showed “esophageal dysmotility”, prompting an esophagus-focused consultation.
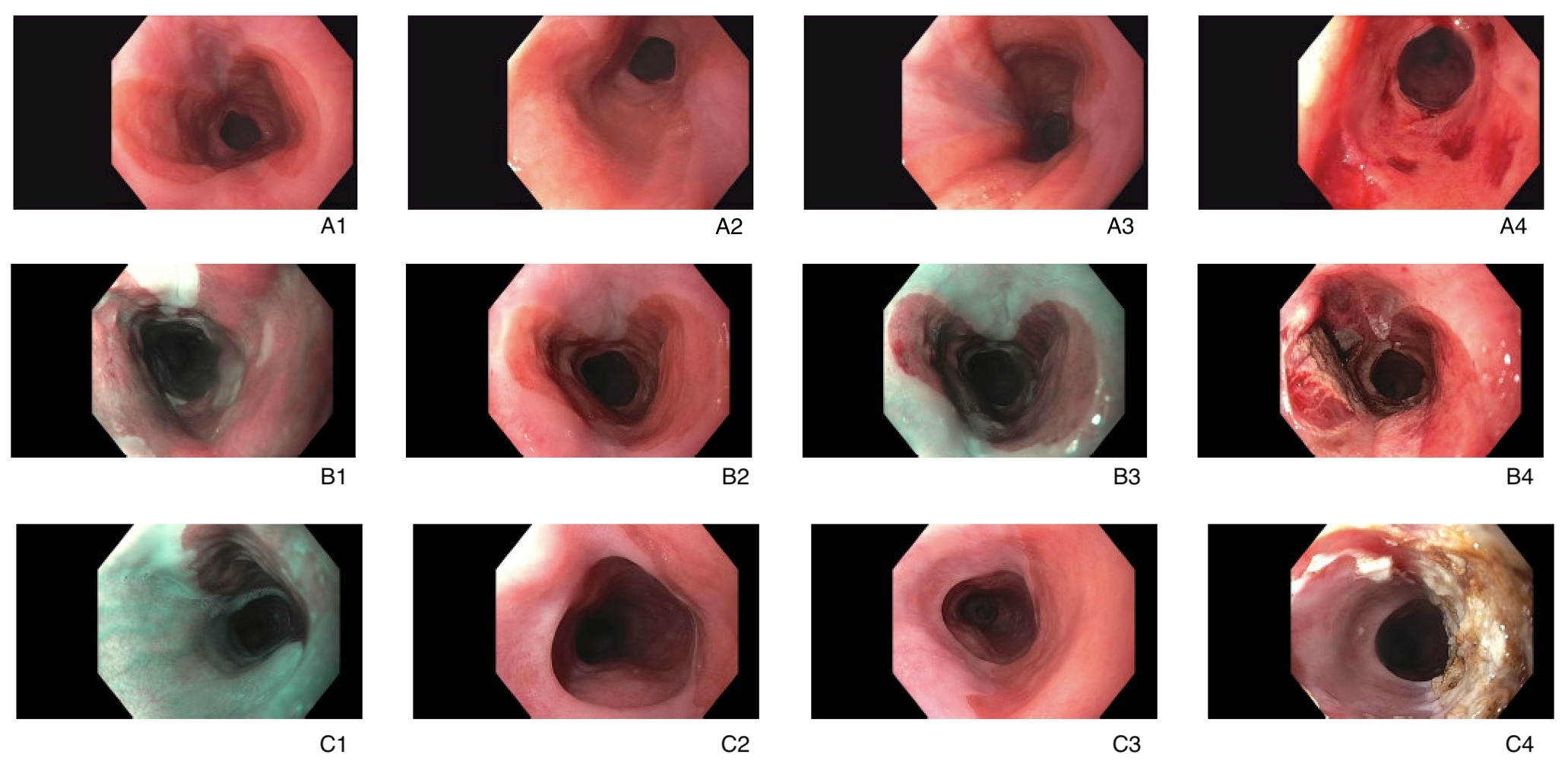
Given the symptoms trajectory and concern for missed eosinophilic esophagitis, repeat EGD was performed. A single large bilobed and circumferential area of salmon-colored mucosa was found in the upper third of the esophagus with adjacent moderate stenosis and the distal margin. Balloon dilation was performed to a diameter of 15 mm, resulting in symptom resolution. Biopsies confirmed this tissue contained gastric mucosa. To prevent further episodes of dysphagia, the patient was started on chronic PPI therapy, and endoscopic ablation was performed to eradicate the CIP. Despite attempts to mitigate recurrent stricture by ablating only one hemi-circumference at a time, the patient developed dysphagia after the second treatment, requiring additional dilation.
Discussion: Acid-secreting CIPs often produce nonspecific symptoms including throat discomfort, globus sensation, odynophagia, and dysphagia. Although rare, mucosal complications such as esophagitis, ulcers, and strictures can develop due to ongoing acid exposure. The CIP detection rate ranges from 1 to 21% in endoscopic studies, but reaches 70% in autopsy studies, suggesting the prevalence is underestimated. Due to its location, a CIP can easily be missed without a deliberate inspection of the proximal esophagus. One study reported that increased awareness of CIP could boost its endoscopic prevalence tenfold. This case suggests a potential benefit to repeating an EGD for persistent solid food dysphagia without manometric or radiographic abnormalities.
Disclosures:
Yuhong Yang, MD1, Michael S.. Smith, MD, MBA2, Kimberly Cavaliere, MD3. P4004 - An Obscure Case of Dysphagia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mount Sinai Beth Israel, Icahn School of Medicine at Mount Sinai, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY; 3Icahn School of Medicine at Mount Sinai Morningside/West, New York, NY
Introduction: Ectopic gastric mucosa may appear anywhere in the gastrointestinal tract. Its most common location is the proximal esophagus, where it is also known as cervical inlet patches (CIP), and most often asymptomatic. However, when parietal cells are present, acid secretion can lead to symptoms and tissue damage. We present a patient with a large area of ectopic gastric mucosa complicated by peptic stricture.
Case Description/Methods: 53-year-old woman presented with ten years of dysphagia. She noted intermittent solid food dysphagia which progressively worsened. She reported a sensation of food remaining in her throat about twice a month, associated with chest pain and difficulty swallowing both water and saliva. Prior evaluation included a normal barium esophagram, upper endoscopy (EGD), and laryngoscopy. Empiric proton pump inhibitor (PPI) and intermittent fasting improved her dysphagia. A subsequent modified barium swallow showed “esophageal dysmotility”, prompting an esophagus-focused consultation.
Given the symptoms trajectory and concern for missed eosinophilic esophagitis, repeat EGD was performed. A single large bilobed and circumferential area of salmon-colored mucosa was found in the upper third of the esophagus with adjacent moderate stenosis and the distal margin. Balloon dilation was performed to a diameter of 15 mm, resulting in symptom resolution. Biopsies confirmed this tissue contained gastric mucosa. To prevent further episodes of dysphagia, the patient was started on chronic PPI therapy, and endoscopic ablation was performed to eradicate the CIP. Despite attempts to mitigate recurrent stricture by ablating only one hemi-circumference at a time, the patient developed dysphagia after the second treatment, requiring additional dilation.
Discussion: Acid-secreting CIPs often produce nonspecific symptoms including throat discomfort, globus sensation, odynophagia, and dysphagia. Although rare, mucosal complications such as esophagitis, ulcers, and strictures can develop due to ongoing acid exposure. The CIP detection rate ranges from 1 to 21% in endoscopic studies, but reaches 70% in autopsy studies, suggesting the prevalence is underestimated. Due to its location, a CIP can easily be missed without a deliberate inspection of the proximal esophagus. One study reported that increased awareness of CIP could boost its endoscopic prevalence tenfold. This case suggests a potential benefit to repeating an EGD for persistent solid food dysphagia without manometric or radiographic abnormalities.
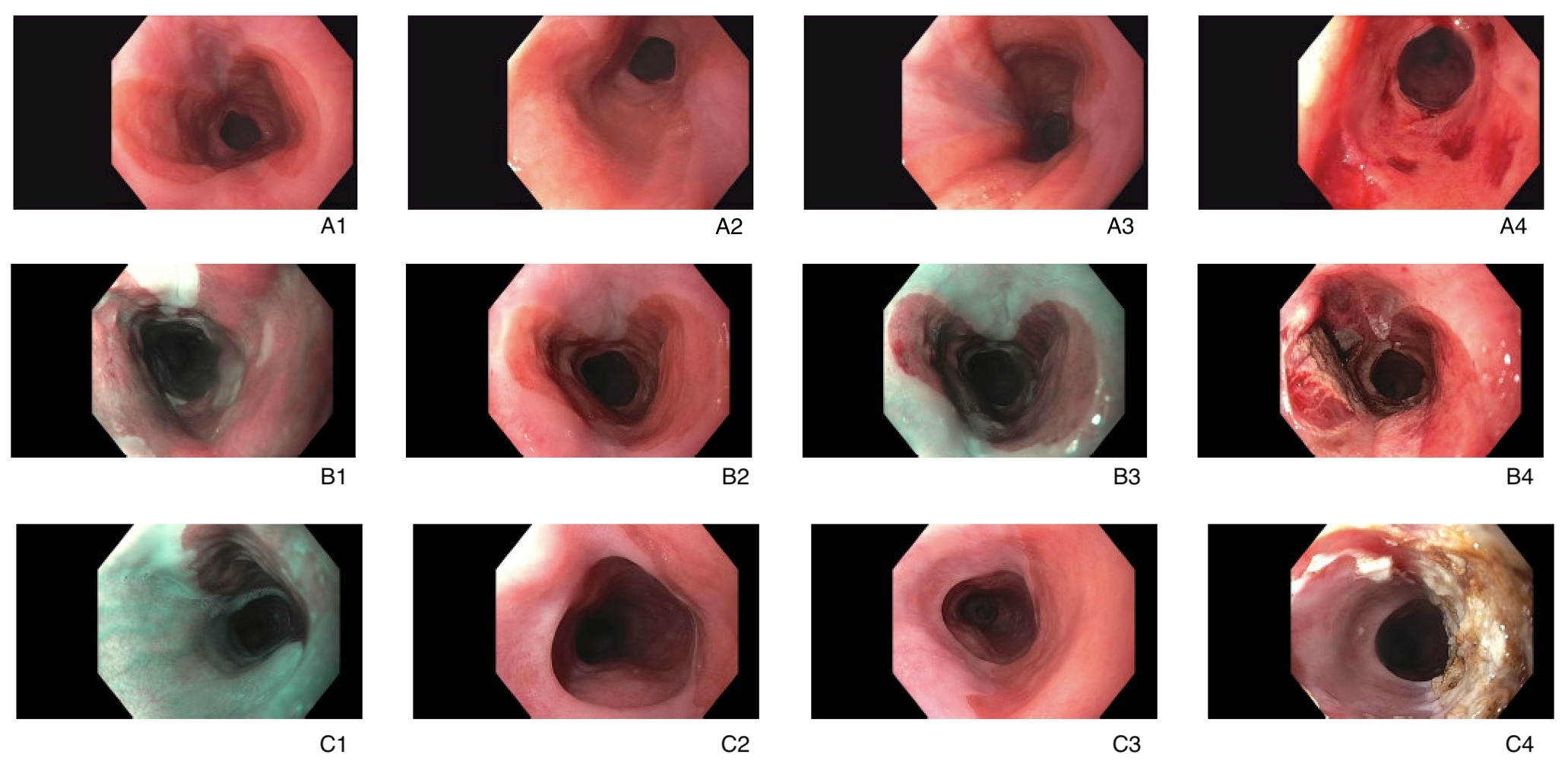
Figure: A1-A4: Pictures from the repeat endoscopy. A1, A2, A3: Upper third of the esophagus, with a large bilobed and circumferential area of salmon-colored mucosa. A4: Upper third of the esophagus post-dilation.
B1-B4: Endoscopy picture from the first treatment. B1, B3: Upper third of the esophagus with inlet patch under narrow-band imaging. B2: Upper third of the esophagus with inlet patch. B4: Upper third of the esophagus post ablation of the left hemi-circumference of the inlet
patch.
C1-C4: Endoscopy picture from the second treatment. C1: Upper third of the esophagus with inlet patch under narrow-band imaging. C2: Upper third of the esophagus with inlet patch and stricture. C3: Upper third of the esophagus with inlet patch. C4: Upper third of the esophagus after argon plasma coagulation ablation
B1-B4: Endoscopy picture from the first treatment. B1, B3: Upper third of the esophagus with inlet patch under narrow-band imaging. B2: Upper third of the esophagus with inlet patch. B4: Upper third of the esophagus post ablation of the left hemi-circumference of the inlet
patch.
C1-C4: Endoscopy picture from the second treatment. C1: Upper third of the esophagus with inlet patch under narrow-band imaging. C2: Upper third of the esophagus with inlet patch and stricture. C3: Upper third of the esophagus with inlet patch. C4: Upper third of the esophagus after argon plasma coagulation ablation
Disclosures:
Yuhong Yang indicated no relevant financial relationships.
Michael Smith: Castle Biosciences – Advisory Committee/Board Member, Consultant. CDx Diagnostics – Consultant. Lucid Diagnostics – Advisory Committee/Board Member, Consultant. Provation Medical – Consultant. Steris Endoscopy – Advisory Committee/Board Member, Consultant.
Kimberly Cavaliere indicated no relevant financial relationships.
Yuhong Yang, MD1, Michael S.. Smith, MD, MBA2, Kimberly Cavaliere, MD3. P4004 - An Obscure Case of Dysphagia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
