Tuesday Poster Session
Category: Esophagus
P4006 - The Devil is in the Details: An Esophageal Inlet Patch Harboring Adenocarcinoma
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Jonathan Ghobrial, MD
Allegheny Health Network Medicine Institute
Pittsburgh, PA
Presenting Author(s)
Chandan Dash, MBBS, MD1, Evan Reinhart, DO2, Manish K. Dhawan, MD2, Jonathan Ghobrial, MD1
1Allegheny Health Network Medicine Institute, Pittsburgh, PA; 2Allegheny Center for Digestive Health, Pittsburgh, PA
Introduction: Heterotopic gastric mucosa in the upper esophagus, commonly known as a cervical inlet patch (IP), is found in 1-10% of the population. 1,2 Inlet patches are commonly asymptomatic and are typically identified incidentally during endoscopy. The detection rate of inlet patches is dependent on the awareness of the endoscopist about the inlet patch during the procedure. 2 In current literature there is a limited understanding of the malignant transformation potential of esophageal inlet patches.
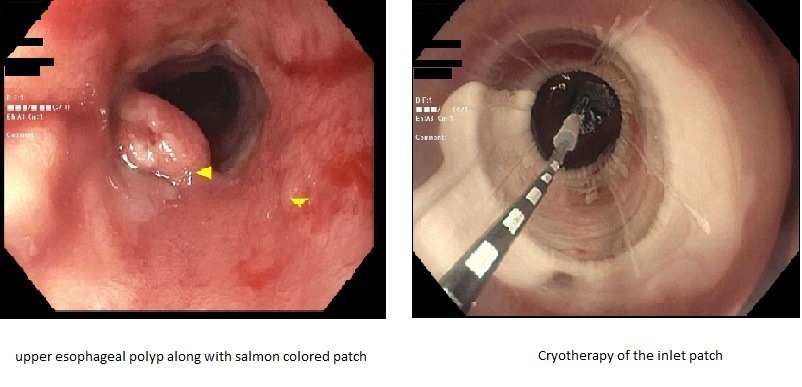
Case Description/Methods: We present a case of a 48 y.o. male with history of hyperlipidemia and irritable bowel syndrome – diarrheal subtype who presented for endoscopic screening of Barrett’s esophagus in the setting of chronic GERD without esophagitis. Initial endoscopy revealed a circumferential salmon colored patch 20-23 cm from the incisors and a single polyp within the salmon-colored patch without any evidence of Barrett’s esophagus near the GE junction. The polyp was excised and biopsies were taken from the salmon-colored patch which showed oxyntic type gastric mucosa consistent with inlet patch, with moderately differentiated intra-mucosal adenocarcinoma arising with in metaplastic epithelium with high grade dysplasia. Repeat EGD was performed which redemonstrated the circumferential salmon-colored patch. EUS revealed an abnormal left upper para-tracheal lymph node. Biopsies taken from the inlet patch did not show any residual malignancy. The patient was treated with proton pump inhibitor. Repeat EUS did not show the abnormal para-tracheal lymph node and patient was treated with partial circumference cryotherapy with plans to treat the remaining part in repeat EGD.
Discussion: On review, patient’s with IP are typically asymptomatic. The common symptomatic presentations include: dysphagia, heart burn and globus sensation likely as a result from local acid production leading to esophagitis, ulcer, web and stricture formation. Serious and life-threatening sequelae such as hemorrhage, perforation, and tracheoesophageal fistula may occur in rare cases. Barrett’s like Intestinal metaplasia with high grade dysplasia and adenocarcinoma arising with in the vicinity of an inlet patch is extremely rare.3 This case demonstrates the importance to be vigilant for the presence of an inlet patch and to conduct a careful examination with sampling in the event mucosal abnormalities are visualized.
Disclosures:
Chandan Dash, MBBS, MD1, Evan Reinhart, DO2, Manish K. Dhawan, MD2, Jonathan Ghobrial, MD1. P4006 - The Devil is in the Details: An Esophageal Inlet Patch Harboring Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Allegheny Health Network Medicine Institute, Pittsburgh, PA; 2Allegheny Center for Digestive Health, Pittsburgh, PA
Introduction: Heterotopic gastric mucosa in the upper esophagus, commonly known as a cervical inlet patch (IP), is found in 1-10% of the population. 1,2 Inlet patches are commonly asymptomatic and are typically identified incidentally during endoscopy. The detection rate of inlet patches is dependent on the awareness of the endoscopist about the inlet patch during the procedure. 2 In current literature there is a limited understanding of the malignant transformation potential of esophageal inlet patches.
Case Description/Methods: We present a case of a 48 y.o. male with history of hyperlipidemia and irritable bowel syndrome – diarrheal subtype who presented for endoscopic screening of Barrett’s esophagus in the setting of chronic GERD without esophagitis. Initial endoscopy revealed a circumferential salmon colored patch 20-23 cm from the incisors and a single polyp within the salmon-colored patch without any evidence of Barrett’s esophagus near the GE junction. The polyp was excised and biopsies were taken from the salmon-colored patch which showed oxyntic type gastric mucosa consistent with inlet patch, with moderately differentiated intra-mucosal adenocarcinoma arising with in metaplastic epithelium with high grade dysplasia. Repeat EGD was performed which redemonstrated the circumferential salmon-colored patch. EUS revealed an abnormal left upper para-tracheal lymph node. Biopsies taken from the inlet patch did not show any residual malignancy. The patient was treated with proton pump inhibitor. Repeat EUS did not show the abnormal para-tracheal lymph node and patient was treated with partial circumference cryotherapy with plans to treat the remaining part in repeat EGD.
Discussion: On review, patient’s with IP are typically asymptomatic. The common symptomatic presentations include: dysphagia, heart burn and globus sensation likely as a result from local acid production leading to esophagitis, ulcer, web and stricture formation. Serious and life-threatening sequelae such as hemorrhage, perforation, and tracheoesophageal fistula may occur in rare cases. Barrett’s like Intestinal metaplasia with high grade dysplasia and adenocarcinoma arising with in the vicinity of an inlet patch is extremely rare.3 This case demonstrates the importance to be vigilant for the presence of an inlet patch and to conduct a careful examination with sampling in the event mucosal abnormalities are visualized.
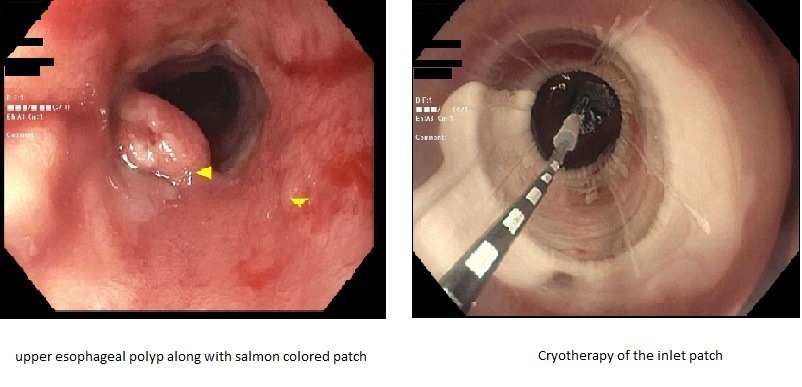
Figure: Initial image of the inlet patch followed by image of the inlet patch after partial thickness cryotherapy
Disclosures:
Chandan Dash indicated no relevant financial relationships.
Evan Reinhart indicated no relevant financial relationships.
Manish Dhawan indicated no relevant financial relationships.
Jonathan Ghobrial indicated no relevant financial relationships.
Chandan Dash, MBBS, MD1, Evan Reinhart, DO2, Manish K. Dhawan, MD2, Jonathan Ghobrial, MD1. P4006 - The Devil is in the Details: An Esophageal Inlet Patch Harboring Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
