Tuesday Poster Session
Category: Esophagus
P4015 - Positive Gastric Emptying Study: Gastroparesis or Achalasia?
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ines Varela, MD
Mount Sinai West, Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Ines Varela Knorr, MD1, Kimberly Cavaliere, MD2
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 2Icahn School of Medicine at Mount Sinai Morningside/West, New York, NY
Introduction: Gastric emptying studies (GES) are tests that have many limitations and can be falsely prolonged in the setting of achalasia. We present three patients in which falsely prolonged GES led to misdiagnosis of gastroparesis as the cause of their symptoms.
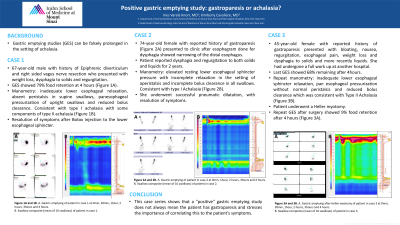
Case Description/Methods: Case 1
67-year-old male with history of epiphrenic diverticulum and right sided vagus nerve resection presented with weight loss, dysphagia to solids and regurgitation. Esophagogastroduodenoscopy (EGD) showed dilation of the lower third of the esophagus. GES was positive. Originally planned for Botox injection to the pylorus and subsequent gastric peroral endoscopic myotomy if successful. However, given EGD findings and dysphagia the patient underwent esophageal manometry which showed achalasia. Consequently, he instead underwent Botox injection to the lower esophageal sphincter. Three months after, the patient’s symptoms had resolved, and he was gaining weight.
Case 2
74-year-old female with reported history of gastroparesis presented to the office after esophagram done for dysphagia showed narrowing of the distal esophagus. Patient reported dysphagia and regurgitation to both solids and liquids for 2 years. EGD showed dilation in the esophagus, hypertonic lower esophageal sphincter and no evidence of mass. Manometry showed Type I Achalasia. She underwent successful pneumatic dilatation, resolving her symptoms entirely.
Case 3
45-year-old female with reported history of gastroparesis presented with bloating, nausea, regurgitation, esophageal pain, weight loss and dysphagia to solids and liquids. Symptoms started in 2018 and she had undergone an extensive work up including positive GES, esophagram concerning for achalasia and equivocal esophageal manometry. Over the years, her symptoms had worsened despite treatment, and she had lost significant weight. She underwent repeat manometry which showed Type II Achalasia. EGD was repeated which ruled out pseudo achalasia and she underwent a Heller myotomy. Two months later her symptoms had resolved. Repeat GES after surgery was negative.
Discussion: A study that looked at postprandial gastric relaxation in achalasia suggested that patients with achalasia might have secondary neural damage extending to the proximal stomach (Bittinger et al. 1998). This case series shows that these patients might have no damage to gastric motility. These false results might be because a dilated esophagus leads to the retention of food in the esophagus mimicking delayed gastric emptying on GES.
Disclosures:
Ines Varela Knorr, MD1, Kimberly Cavaliere, MD2. P4015 - Positive Gastric Emptying Study: Gastroparesis or Achalasia?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 2Icahn School of Medicine at Mount Sinai Morningside/West, New York, NY
Introduction: Gastric emptying studies (GES) are tests that have many limitations and can be falsely prolonged in the setting of achalasia. We present three patients in which falsely prolonged GES led to misdiagnosis of gastroparesis as the cause of their symptoms.
Case Description/Methods: Case 1
67-year-old male with history of epiphrenic diverticulum and right sided vagus nerve resection presented with weight loss, dysphagia to solids and regurgitation. Esophagogastroduodenoscopy (EGD) showed dilation of the lower third of the esophagus. GES was positive. Originally planned for Botox injection to the pylorus and subsequent gastric peroral endoscopic myotomy if successful. However, given EGD findings and dysphagia the patient underwent esophageal manometry which showed achalasia. Consequently, he instead underwent Botox injection to the lower esophageal sphincter. Three months after, the patient’s symptoms had resolved, and he was gaining weight.
Case 2
74-year-old female with reported history of gastroparesis presented to the office after esophagram done for dysphagia showed narrowing of the distal esophagus. Patient reported dysphagia and regurgitation to both solids and liquids for 2 years. EGD showed dilation in the esophagus, hypertonic lower esophageal sphincter and no evidence of mass. Manometry showed Type I Achalasia. She underwent successful pneumatic dilatation, resolving her symptoms entirely.
Case 3
45-year-old female with reported history of gastroparesis presented with bloating, nausea, regurgitation, esophageal pain, weight loss and dysphagia to solids and liquids. Symptoms started in 2018 and she had undergone an extensive work up including positive GES, esophagram concerning for achalasia and equivocal esophageal manometry. Over the years, her symptoms had worsened despite treatment, and she had lost significant weight. She underwent repeat manometry which showed Type II Achalasia. EGD was repeated which ruled out pseudo achalasia and she underwent a Heller myotomy. Two months later her symptoms had resolved. Repeat GES after surgery was negative.
Discussion: A study that looked at postprandial gastric relaxation in achalasia suggested that patients with achalasia might have secondary neural damage extending to the proximal stomach (Bittinger et al. 1998). This case series shows that these patients might have no damage to gastric motility. These false results might be because a dilated esophagus leads to the retention of food in the esophagus mimicking delayed gastric emptying on GES.
Disclosures:
Ines Varela Knorr indicated no relevant financial relationships.
Kimberly Cavaliere indicated no relevant financial relationships.
Ines Varela Knorr, MD1, Kimberly Cavaliere, MD2. P4015 - Positive Gastric Emptying Study: Gastroparesis or Achalasia?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
