Tuesday Poster Session
Category: Esophagus
P4020 - Melanoma is More Than Skin Deep: A Rare Case of Primary Melanoma of the Esophagus
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Mansi Sheth, DO
Jefferson Torresdale Hospital
Bridgewater, NJ
Presenting Author(s)
Mansi Sheth, DO1, Seth Lipshutz, DO2, Marisa Pope, DO3, Tehilla Apfel, MD1, Katelyn Phelps, DO1
1Jefferson Torresdale Hospital, Philadelphia, PA; 2Jefferson Health, Ivyland, PA; 3Jefferson Health, Washington Township, NJ
Introduction: Melanoma is a very well-known deadly cancer commonly associated with primary lesions of the epidermis. Primary malignant melanoma of the esophagus (PMME) accounts for less than 0.05% of all melanoma cases. We report a rare case of a primary malignant melanoma of the esophagus.
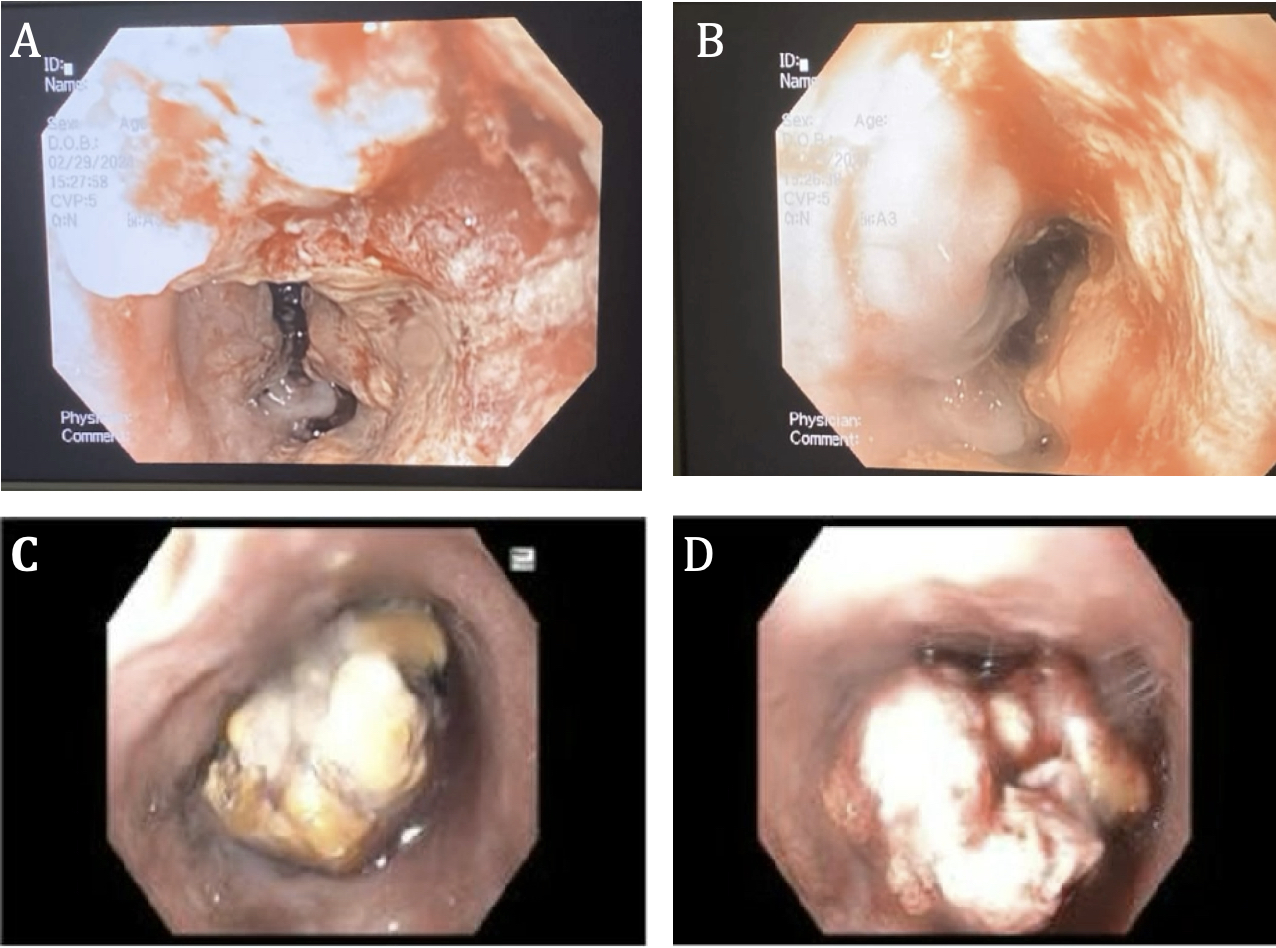
Case Description/Methods: Patient is a 65-year-old male with past medical history of hypertension, type 2 diabetes, and alcohol abuse who presented after a motor vehicle accident, and was found to have slurred speech, confusion, and emesis. He underwent a full body CT scan and was noted to have a severely dilated esophagus from diaphragm to cervical spine filled with fluid and food. The patient was admitted for sepsis and altered mental status and was eventually upgraded to the ICU for respiratory distress requiring intubation. While in the ICU, he underwent an esophogastroduodenoscopy (EGD) which found retained food and fluid, abnormal appearing esophageal mucosa with diffuse ulcerations concerning for malignancy, and inability to transverse into the stomach. Biopsies were positive for malignant melanoma. He underwent a follow-up EGD with findings of a fungating ulcerative mass with pigmentation (Image 1) and normal stomach and duodenum. Oncology believed the lesion was metastatic from a cutaneous lesion, however, no specific skin lesions were found, and as no additional evidence of metastasis was seen throughout the body, it was presumed that the patient had PMME. The tumor was positive for vimentin, S100, and SOX10 on immunohistochemical staining. He had an extensive hospital course complicated by respiratory distress requiring intubation, pleural effusions requiring chest tube placement, pneumatosis intestinalis, bowel ischemia and multisystem organ failure which led to his demise.
Discussion: PMME is rare and accounts for 0.1-0.2% of esophageal tumors. Diagnosis is often delayed as patients present with nonspecific symptoms like dysphagia and epigastric pain. EGD reveals tumor growth predominantly in the lower esophagus. Biopsies show evidence of melanocytosis in up to 30% of PMME samples, therefore immunohistochemical studies are required to confirm the diagnosis. Melanosis is thought to be due to chronic esophagitis or hyperplastic epithelium. In our patient, melanosis may have been associated with heavy alcohol use leading to esophagitis. Our case of an incidentally found PMME highlights the importance of early detection, and offers a potential link between alcohol use-related esophagitis and its development.
Disclosures:
Mansi Sheth, DO1, Seth Lipshutz, DO2, Marisa Pope, DO3, Tehilla Apfel, MD1, Katelyn Phelps, DO1. P4020 - Melanoma is More Than Skin Deep: A Rare Case of Primary Melanoma of the Esophagus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Jefferson Torresdale Hospital, Philadelphia, PA; 2Jefferson Health, Ivyland, PA; 3Jefferson Health, Washington Township, NJ
Introduction: Melanoma is a very well-known deadly cancer commonly associated with primary lesions of the epidermis. Primary malignant melanoma of the esophagus (PMME) accounts for less than 0.05% of all melanoma cases. We report a rare case of a primary malignant melanoma of the esophagus.
Case Description/Methods: Patient is a 65-year-old male with past medical history of hypertension, type 2 diabetes, and alcohol abuse who presented after a motor vehicle accident, and was found to have slurred speech, confusion, and emesis. He underwent a full body CT scan and was noted to have a severely dilated esophagus from diaphragm to cervical spine filled with fluid and food. The patient was admitted for sepsis and altered mental status and was eventually upgraded to the ICU for respiratory distress requiring intubation. While in the ICU, he underwent an esophogastroduodenoscopy (EGD) which found retained food and fluid, abnormal appearing esophageal mucosa with diffuse ulcerations concerning for malignancy, and inability to transverse into the stomach. Biopsies were positive for malignant melanoma. He underwent a follow-up EGD with findings of a fungating ulcerative mass with pigmentation (Image 1) and normal stomach and duodenum. Oncology believed the lesion was metastatic from a cutaneous lesion, however, no specific skin lesions were found, and as no additional evidence of metastasis was seen throughout the body, it was presumed that the patient had PMME. The tumor was positive for vimentin, S100, and SOX10 on immunohistochemical staining. He had an extensive hospital course complicated by respiratory distress requiring intubation, pleural effusions requiring chest tube placement, pneumatosis intestinalis, bowel ischemia and multisystem organ failure which led to his demise.
Discussion: PMME is rare and accounts for 0.1-0.2% of esophageal tumors. Diagnosis is often delayed as patients present with nonspecific symptoms like dysphagia and epigastric pain. EGD reveals tumor growth predominantly in the lower esophagus. Biopsies show evidence of melanocytosis in up to 30% of PMME samples, therefore immunohistochemical studies are required to confirm the diagnosis. Melanosis is thought to be due to chronic esophagitis or hyperplastic epithelium. In our patient, melanosis may have been associated with heavy alcohol use leading to esophagitis. Our case of an incidentally found PMME highlights the importance of early detection, and offers a potential link between alcohol use-related esophagitis and its development.
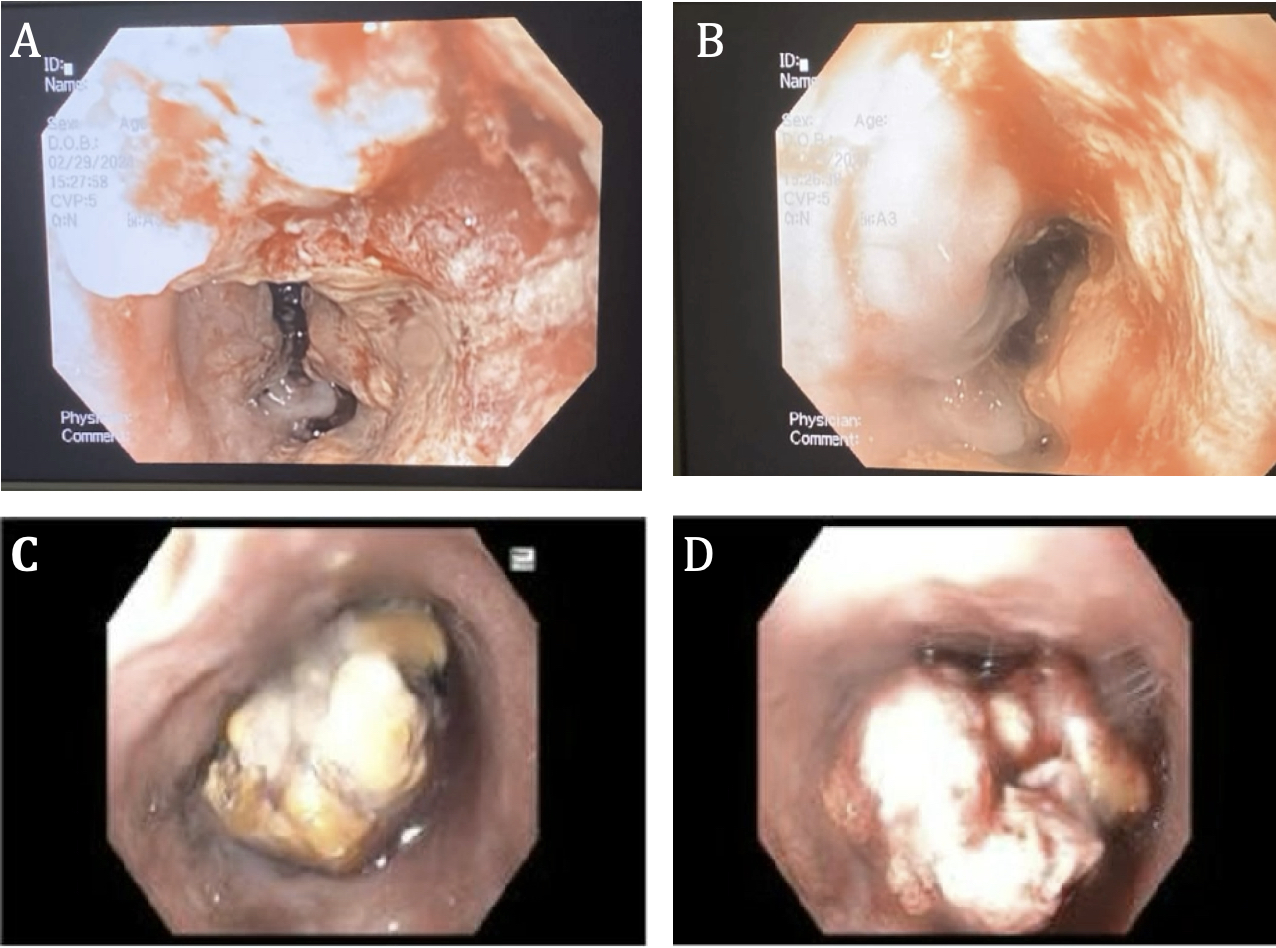
Figure: Image 1. A. Initial EGD at bedside showing erosions and ulceration of the esophagus. B. Initial EGD at bedside showing diffuse erosions. C. Subsequent EGD showing a fungating mass in the GE junction. D. Subsequent EGD showing a fungating mass in the GE junction.
Disclosures:
Mansi Sheth indicated no relevant financial relationships.
Seth Lipshutz indicated no relevant financial relationships.
Marisa Pope indicated no relevant financial relationships.
Tehilla Apfel indicated no relevant financial relationships.
Katelyn Phelps indicated no relevant financial relationships.
Mansi Sheth, DO1, Seth Lipshutz, DO2, Marisa Pope, DO3, Tehilla Apfel, MD1, Katelyn Phelps, DO1. P4020 - Melanoma is More Than Skin Deep: A Rare Case of Primary Melanoma of the Esophagus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

