Tuesday Poster Session
Category: Esophagus
P4034 - Lymphocytic Esophagitis: A Zebra Diagnosis Associated With Noncardiac Chest Pain
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Martin Ankamah, MBA
University of St. Thomas Houston
Houston, TX
Presenting Author(s)
Martin Ankamah, MBA1, Robert S.. Aaron, MD2
1University of St. Thomas Houston, Houston, TX; 2Allied Digestive Health (Middlesex Monmouth Gastroenterology), Freehold, NJ
Introduction: The first publication on lymphocytic esophagitis (LyE) was published in 2006, and still much remains unknown about this uncommon disease. It is characterized by three histologic features: intraepithelial lymphocytosis predominately around peripapillary fields, an absence or low count of neutrophils and eosinophils, and evidence of epithelial damage most frequently in the form of intercellular edema. Endoscopic findings may appear normal but can include strictures, plaques, rings, or furrows. Dysphagia is the most common symptom, and some patients experience reflux, chest pain, nausea, or vomiting. There is no standardized treatment for LyE. In some studies, patients have responded well to proton pump inhibitors or corticosteroids. By sharing this clinical vignette, the objective is to further the understanding of this rare disease.
Case Description/Methods: The patient is a 73-year-old man with a past medical history significant for chronic GERD (on longstanding PPI therapy) and a remote history of coronary artery disease requiring cardiac stenting in 2012. He was evaluated in the office for noncardiac chest pain and abdominal bloating prompting a hospital admission. Physical examination was unremarkable. Upper endoscopy demonstrated a normal appearing esophagus, multiple small fundic gland polyps, and patchy antral erythema. Biopsies taken of both the mid and distal esophagus were demonstrative of lymphocytic esophagitis. Gastric biopsies demonstrated mild chronic gastritis without evidence of H. pylori or intestinal metaplasia. Duodenal biopsies were negative for celiac disease.
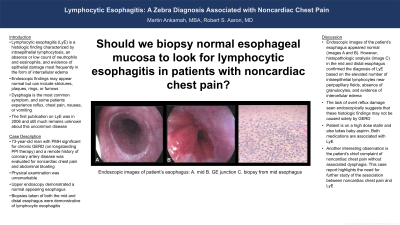
Discussion: Endoscopic images of the patient’s esophagus appeared normal (images A and B). However, histopathologic analysis (image C) in the mid and distal esophagus confirmed the diagnosis of LyE based on the elevated number of intraepithelial lymphocytes near peripapillary fields, absence of granulocytes, and evidence of intercellular edema. The lack of overt reflux damage seen endoscopically suggests that these histologic findings may not be caused solely by GERD. The patient is on a high dose statin and also takes baby aspirin. Both medications are associated with LyE. Another interesting observation is the patient’s chief complaint of noncardiac chest pain without associated dysphagia. This case report highlights the need for further study of the association between noncardiac chest pain and LyE.

Disclosures:
Martin Ankamah, MBA1, Robert S.. Aaron, MD2. P4034 - Lymphocytic Esophagitis: A Zebra Diagnosis Associated With Noncardiac Chest Pain, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of St. Thomas Houston, Houston, TX; 2Allied Digestive Health (Middlesex Monmouth Gastroenterology), Freehold, NJ
Introduction: The first publication on lymphocytic esophagitis (LyE) was published in 2006, and still much remains unknown about this uncommon disease. It is characterized by three histologic features: intraepithelial lymphocytosis predominately around peripapillary fields, an absence or low count of neutrophils and eosinophils, and evidence of epithelial damage most frequently in the form of intercellular edema. Endoscopic findings may appear normal but can include strictures, plaques, rings, or furrows. Dysphagia is the most common symptom, and some patients experience reflux, chest pain, nausea, or vomiting. There is no standardized treatment for LyE. In some studies, patients have responded well to proton pump inhibitors or corticosteroids. By sharing this clinical vignette, the objective is to further the understanding of this rare disease.
Case Description/Methods: The patient is a 73-year-old man with a past medical history significant for chronic GERD (on longstanding PPI therapy) and a remote history of coronary artery disease requiring cardiac stenting in 2012. He was evaluated in the office for noncardiac chest pain and abdominal bloating prompting a hospital admission. Physical examination was unremarkable. Upper endoscopy demonstrated a normal appearing esophagus, multiple small fundic gland polyps, and patchy antral erythema. Biopsies taken of both the mid and distal esophagus were demonstrative of lymphocytic esophagitis. Gastric biopsies demonstrated mild chronic gastritis without evidence of H. pylori or intestinal metaplasia. Duodenal biopsies were negative for celiac disease.
Discussion: Endoscopic images of the patient’s esophagus appeared normal (images A and B). However, histopathologic analysis (image C) in the mid and distal esophagus confirmed the diagnosis of LyE based on the elevated number of intraepithelial lymphocytes near peripapillary fields, absence of granulocytes, and evidence of intercellular edema. The lack of overt reflux damage seen endoscopically suggests that these histologic findings may not be caused solely by GERD. The patient is on a high dose statin and also takes baby aspirin. Both medications are associated with LyE. Another interesting observation is the patient’s chief complaint of noncardiac chest pain without associated dysphagia. This case report highlights the need for further study of the association between noncardiac chest pain and LyE.

Figure: Endoscopic images of patient’s esophagus: A. mid B. GE junction. C. biopsy from mid esophagus
Disclosures:
Martin Ankamah indicated no relevant financial relationships.
Robert Aaron indicated no relevant financial relationships.
Martin Ankamah, MBA1, Robert S.. Aaron, MD2. P4034 - Lymphocytic Esophagitis: A Zebra Diagnosis Associated With Noncardiac Chest Pain, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
