Tuesday Poster Session
Category: Functional Bowel Disease
P4041 - Auricular Neurostimulation Improves Abdominal Pain, Nausea, Psychological Functioning, and Sleep in Patients Over 18 Years of Age
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio
- AV
Austin VonAxelson, MD
University of Cincinnati College of Medicine
Cincinnati, OH
Presenting Author(s)
Austin VonAxelson, MD1, Neha Santucci, MD2, Umber Waheed, MD2, Khalil El-Chamas, MD2, Kahleb Graham, MD2, Jennifer Hardy, MS2, Megan Miller, PhD2, Rashmi Sahay, PhD2, Lin Fei, PhD2
1University of Cincinnati College of Medicine, Cincinnati, OH; 2Cincinnati Children's Hospital Medical Center, Cincinnati, OH
Introduction: Disorders of gut-brain interaction (DGBI) affect nearly 40% of the population and are often associated with adverse symptoms and diminished psychological functioning. Percutaneous electrical nerve field stimulation (PENFS), a minimally invasive, non-pharmacologic approach, improves symptoms in children with DGBI by modulating central pain pathways through auricular branches of cranial nerves supplying the gut. We analyzed outcomes for DGBI patients over 18y undergoing PENFS.
Methods: We retrospectively reviewed charts of 70 patients with DGBI >18y of age, who met the Rome 4 criteria for a DGBI and underwent PENFS at Cincinnati Children’s Hospital. We excluded organic gastrointestinal and systemic conditions. We included demographic data and validated questionnaire responses routinely used in clinical care during 4 weeks of treatment: Abdominal Pain Index, Nausea Severity Scale, Pain Catastrophizing Scale - Children , Children’s Somatization Inventory, Screen for Child Anxiety Related Disorders, Functional Disability Inventory, Pediatric Insomnia Severity Index, and Patient Health Questionnaire Depression Scale. We compared their results with a group of children with similar inclusion criteria younger than 18y.
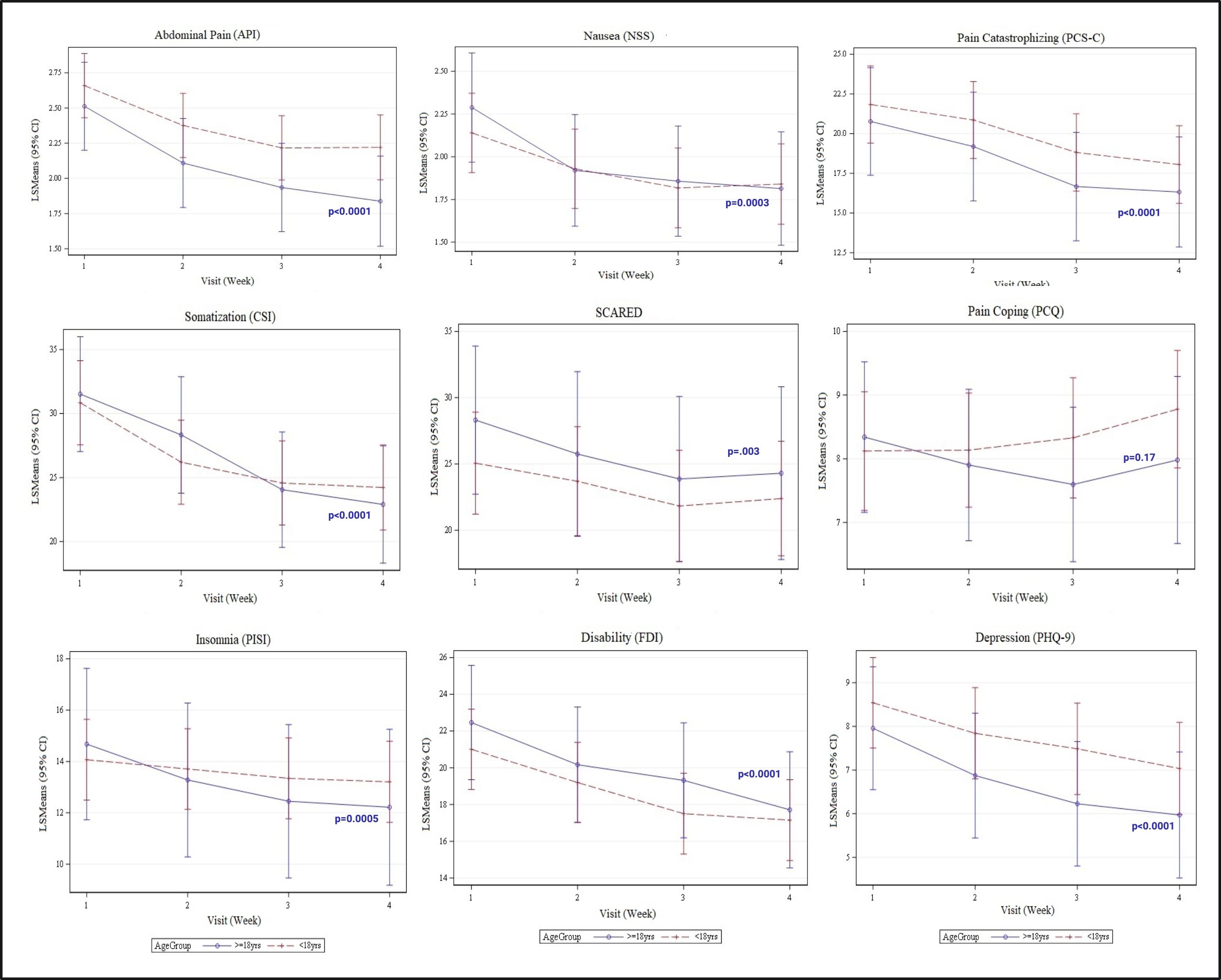
Results: The >18y group included 70 patients [mean age 19.1 ± 1.7y (18-28y), 77% female, 89% Caucasian)]. Irritable bowel syndrome (59%) was the most common diagnosis followed by functional dyspepsia (46%), functional abdominal pain (17%), functional nausea/vomiting (17%), rumination (6%) and abdominal migraine (1%). Abdominal Pain Index, Nausea Severity Scale,Pain Catastrophizing Scale - Children, Functional Disability Inventory, Pediatric Insomnia Severity Index, Children’s Somatization Inventory, Screen for Child Anxiety Related Disorders and Patient Health Questionnaire scores improved after treatment (p< 0.05, figure 1). In comparison with 165 patients < 18y [mean age 14.9 ± 2y (13-17y), 77% female, 87% Caucasian), there was no difference in response at any time point during treatment with >18y (p >0.05).
Discussion: PENFS improved nausea, abdominal pain, pain catastrophizing, sleep disturbances, anxiety, depression and functioning in DGBI patients over 18y of age similar to younger children. The benefits of PENFS in patients under 18 years are well established and have broad applications. This displays that PENFS may be an additional, minimally invasive, non-pharmacologic treatment modality for adult patients with DGBI. Thus, PENFS warrants further exploration of its potential utility in the adult population of patients with DGBI.
Disclosures:
Austin VonAxelson, MD1, Neha Santucci, MD2, Umber Waheed, MD2, Khalil El-Chamas, MD2, Kahleb Graham, MD2, Jennifer Hardy, MS2, Megan Miller, PhD2, Rashmi Sahay, PhD2, Lin Fei, PhD2. P4041 - Auricular Neurostimulation Improves Abdominal Pain, Nausea, Psychological Functioning, and Sleep in Patients Over 18 Years of Age, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Cincinnati College of Medicine, Cincinnati, OH; 2Cincinnati Children's Hospital Medical Center, Cincinnati, OH
Introduction: Disorders of gut-brain interaction (DGBI) affect nearly 40% of the population and are often associated with adverse symptoms and diminished psychological functioning. Percutaneous electrical nerve field stimulation (PENFS), a minimally invasive, non-pharmacologic approach, improves symptoms in children with DGBI by modulating central pain pathways through auricular branches of cranial nerves supplying the gut. We analyzed outcomes for DGBI patients over 18y undergoing PENFS.
Methods: We retrospectively reviewed charts of 70 patients with DGBI >18y of age, who met the Rome 4 criteria for a DGBI and underwent PENFS at Cincinnati Children’s Hospital. We excluded organic gastrointestinal and systemic conditions. We included demographic data and validated questionnaire responses routinely used in clinical care during 4 weeks of treatment: Abdominal Pain Index, Nausea Severity Scale, Pain Catastrophizing Scale - Children , Children’s Somatization Inventory, Screen for Child Anxiety Related Disorders, Functional Disability Inventory, Pediatric Insomnia Severity Index, and Patient Health Questionnaire Depression Scale. We compared their results with a group of children with similar inclusion criteria younger than 18y.
Results: The >18y group included 70 patients [mean age 19.1 ± 1.7y (18-28y), 77% female, 89% Caucasian)]. Irritable bowel syndrome (59%) was the most common diagnosis followed by functional dyspepsia (46%), functional abdominal pain (17%), functional nausea/vomiting (17%), rumination (6%) and abdominal migraine (1%). Abdominal Pain Index, Nausea Severity Scale,Pain Catastrophizing Scale - Children, Functional Disability Inventory, Pediatric Insomnia Severity Index, Children’s Somatization Inventory, Screen for Child Anxiety Related Disorders and Patient Health Questionnaire scores improved after treatment (p< 0.05, figure 1). In comparison with 165 patients < 18y [mean age 14.9 ± 2y (13-17y), 77% female, 87% Caucasian), there was no difference in response at any time point during treatment with >18y (p >0.05).
Discussion: PENFS improved nausea, abdominal pain, pain catastrophizing, sleep disturbances, anxiety, depression and functioning in DGBI patients over 18y of age similar to younger children. The benefits of PENFS in patients under 18 years are well established and have broad applications. This displays that PENFS may be an additional, minimally invasive, non-pharmacologic treatment modality for adult patients with DGBI. Thus, PENFS warrants further exploration of its potential utility in the adult population of patients with DGBI.
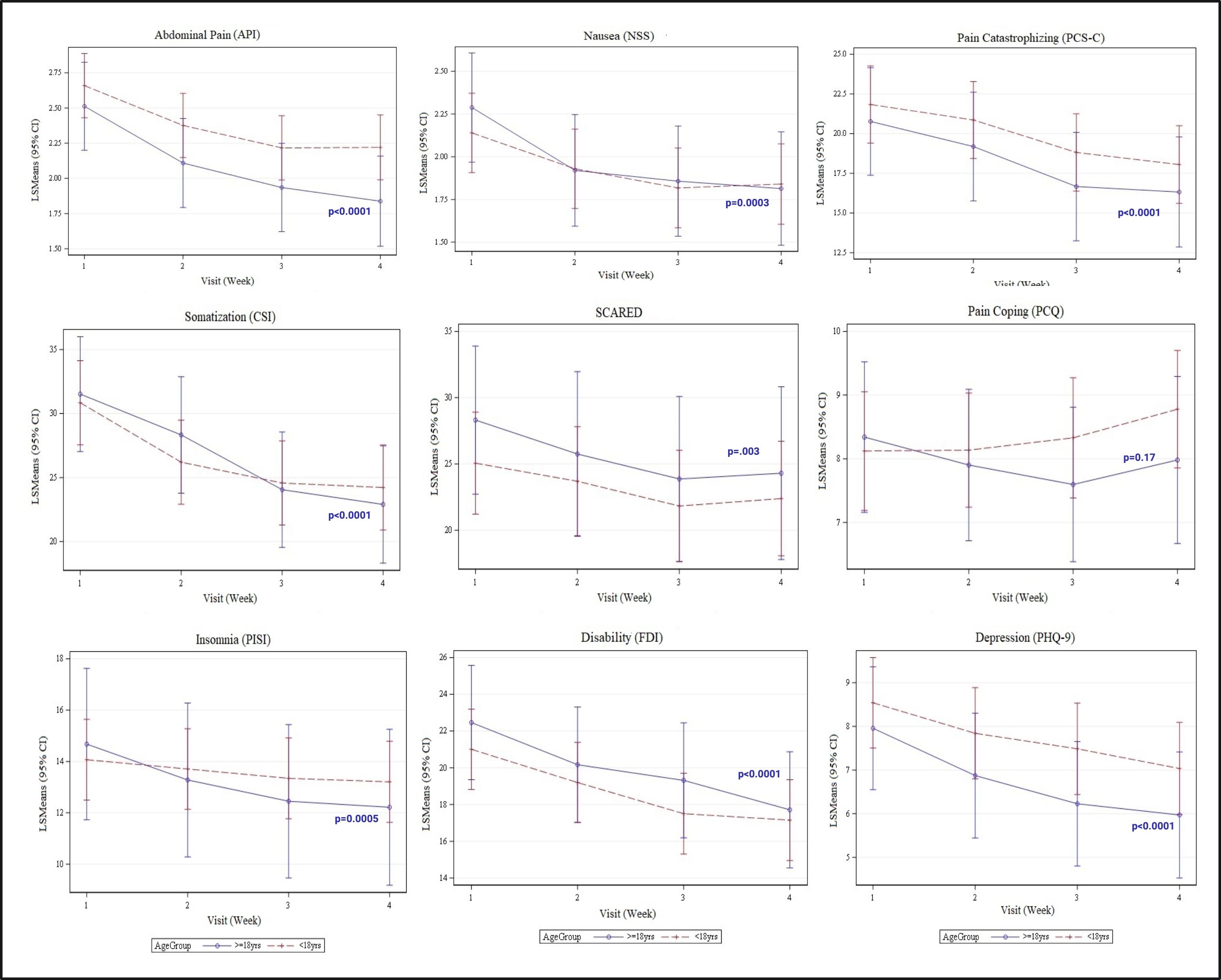
Figure: Figure 1. Validated Outcome Responses over 4 weeks of PENFS
* p-value denotes change in outcomes for patients >18y
Abdominal Pain Index (API), Nausea Severity Scale (NSS), Pain Catastrophizing Scale - Children (PCS-C), Children’s Somatization Inventory (CSI), Screen for Child Anxiety Related Disorders (SCARED), Pain Coping Questionnaire (PCQ), Pediatric Insomnia Severity Index (PISI), Functional Disability Inventory (FDI), and Patient Health Questionnaire (PHQ-9) Depression Scale
* p-value denotes change in outcomes for patients >18y
Abdominal Pain Index (API), Nausea Severity Scale (NSS), Pain Catastrophizing Scale - Children (PCS-C), Children’s Somatization Inventory (CSI), Screen for Child Anxiety Related Disorders (SCARED), Pain Coping Questionnaire (PCQ), Pediatric Insomnia Severity Index (PISI), Functional Disability Inventory (FDI), and Patient Health Questionnaire (PHQ-9) Depression Scale
Disclosures:
Austin VonAxelson indicated no relevant financial relationships.
Neha Santucci: Kate Farms – Key Opinion Leader.
Umber Waheed indicated no relevant financial relationships.
Khalil El-Chamas: Neuraxis – Consultant.
Kahleb Graham indicated no relevant financial relationships.
Jennifer Hardy indicated no relevant financial relationships.
Megan Miller indicated no relevant financial relationships.
Rashmi Sahay indicated no relevant financial relationships.
Lin Fei indicated no relevant financial relationships.
Austin VonAxelson, MD1, Neha Santucci, MD2, Umber Waheed, MD2, Khalil El-Chamas, MD2, Kahleb Graham, MD2, Jennifer Hardy, MS2, Megan Miller, PhD2, Rashmi Sahay, PhD2, Lin Fei, PhD2. P4041 - Auricular Neurostimulation Improves Abdominal Pain, Nausea, Psychological Functioning, and Sleep in Patients Over 18 Years of Age, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
