Tuesday Poster Session
Category: Functional Bowel Disease
P4080 - Diagnostic and Therapeutic Challenges in Hypereosinophilic Syndrome
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Reid Gordon, BS
Wayne State University School of Medicine
Oak Park, MI
Presenting Author(s)
Reid Gordon, BS1, Taha Ashraf, MD2, Syed-Mohammed Jafri, MD2
1Wayne State University School of Medicine, Oak Park, MI; 2Henry Ford Health, Detroit, MI
Introduction: Hypereosinophilic syndrome (HES) is a heterogeneous group of disorders characterized by sustained overproduction of eosinophils. Normally involved in responses to parasites and allergens, excessive eosinophils can cause tissue infiltration and organ damage. We present a case of an adult woman with asthma, allergies, and reflux, presenting with abdominal pain and ascites.
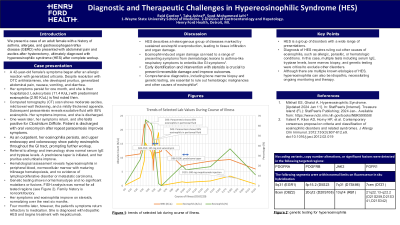
Case Description/Methods: A 42-year-old woman's symptoms began after an allergic reaction with generalized urticaria. Despite resolution with antihistamines, she developed severe pruritus, generalized abdominal pain, nausea, vomiting, and diarrhea. Her symptoms continued to persist one month later and she was ultimately hospitalized. Her white blood count was noted to be elevated at 22.0x10/L with predominant eosinophils at 8.80x109/L. Computed tomography scan shows moderate ascites, mild bowel wall thickening, and a mildly thickened appendix. Subsequent paracentesis reveals exudative fluid with 85% eosinophils. She tested positive for Clostridium Difficile and started oral vancomycin. Upper endoscopy and colonoscopy showed patchy eosinophils throughout the gastrointestinal tract. Her abdominal pain and diarrhea improves and she is discharged home. As an outpatient, her eosinophilia increases to 15.31x109/L, prompting referral to an allergist and immunologist. Normal serum IgE and tryptase levels ruled out common allergic and mast cell disorders. A prednisone taper is initiated, improving her pruritus and urticaria. Hematological assessment reveals hypereosinophilia in peripheral blood, normocellular marrow with maturing trilineage hematopoiesis, and no evidence of lymphoproliferative disorder or metastatic carcinoma. Genetic testing shows normal karyotype and no significant mutations or fusions. Fluorescence in situ hybridization analysis was normal for all tested regions. Family history is noncontributory.<br>Her symptoms and eosinophilia improve on steroids, normalizing over the next 6 months. However, 4 months later, the patient develops recurrent abdominal pain and nausea refractory to medication. She is diagnosed with idiopathic HES and begins treatment with mepolizumab.
Discussion: HES is marked by sustained eosinophil overproduction, leading to organ damage. Early identification and intervention are crucial to prevent irreversible damage and improve outcomes. Comprehensive diagnostics, including bone marrow biopsy and genetic testing, are essential to rule out hematologic malignancies and other causes of eosinophilia.
Disclosures:
Reid Gordon, BS1, Taha Ashraf, MD2, Syed-Mohammed Jafri, MD2. P4080 - Diagnostic and Therapeutic Challenges in Hypereosinophilic Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Wayne State University School of Medicine, Oak Park, MI; 2Henry Ford Health, Detroit, MI
Introduction: Hypereosinophilic syndrome (HES) is a heterogeneous group of disorders characterized by sustained overproduction of eosinophils. Normally involved in responses to parasites and allergens, excessive eosinophils can cause tissue infiltration and organ damage. We present a case of an adult woman with asthma, allergies, and reflux, presenting with abdominal pain and ascites.
Case Description/Methods: A 42-year-old woman's symptoms began after an allergic reaction with generalized urticaria. Despite resolution with antihistamines, she developed severe pruritus, generalized abdominal pain, nausea, vomiting, and diarrhea. Her symptoms continued to persist one month later and she was ultimately hospitalized. Her white blood count was noted to be elevated at 22.0x10/L with predominant eosinophils at 8.80x109/L. Computed tomography scan shows moderate ascites, mild bowel wall thickening, and a mildly thickened appendix. Subsequent paracentesis reveals exudative fluid with 85% eosinophils. She tested positive for Clostridium Difficile and started oral vancomycin. Upper endoscopy and colonoscopy showed patchy eosinophils throughout the gastrointestinal tract. Her abdominal pain and diarrhea improves and she is discharged home. As an outpatient, her eosinophilia increases to 15.31x109/L, prompting referral to an allergist and immunologist. Normal serum IgE and tryptase levels ruled out common allergic and mast cell disorders. A prednisone taper is initiated, improving her pruritus and urticaria. Hematological assessment reveals hypereosinophilia in peripheral blood, normocellular marrow with maturing trilineage hematopoiesis, and no evidence of lymphoproliferative disorder or metastatic carcinoma. Genetic testing shows normal karyotype and no significant mutations or fusions. Fluorescence in situ hybridization analysis was normal for all tested regions. Family history is noncontributory.<br>Her symptoms and eosinophilia improve on steroids, normalizing over the next 6 months. However, 4 months later, the patient develops recurrent abdominal pain and nausea refractory to medication. She is diagnosed with idiopathic HES and begins treatment with mepolizumab.
Discussion: HES is marked by sustained eosinophil overproduction, leading to organ damage. Early identification and intervention are crucial to prevent irreversible damage and improve outcomes. Comprehensive diagnostics, including bone marrow biopsy and genetic testing, are essential to rule out hematologic malignancies and other causes of eosinophilia.
Disclosures:
Reid Gordon indicated no relevant financial relationships.
Taha Ashraf indicated no relevant financial relationships.
Syed-Mohammed Jafri: Gilead, Takeda, Abbvie, Intercept, VectivBio – Advisor or Review Panel Member, Speakers Bureau.
Reid Gordon, BS1, Taha Ashraf, MD2, Syed-Mohammed Jafri, MD2. P4080 - Diagnostic and Therapeutic Challenges in Hypereosinophilic Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
