Tuesday Poster Session
Category: General Endoscopy
P4082 - Will a Visual Aid Improve Colonoscopy Bowel Preparation in Hospitalized Patients? A Pilot Study
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Anagha S. Nagaraj, MD
Montefiore Medical Center, Albert Einstein College of Medicine
Presenting Author(s)
Anagha S. Nagaraj, MD1, Nicholas Costable, MD1, Shawneen Blaize, RN2, Emma Geraghty, RN2, Melissa Fazzari, PhD, MS1, Brett E. Fortune, MD, MS1, Harold Schwartz, MD1, Clara Y. Tow, MD1
1Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY; 2Montefiore Medical Center, Bronx, NY
Introduction: Poor colonoscopy bowel preparation is a common and costly barrier to effective inpatient care. Prior studies have validated a visual aid (VA) as a tool for patient self-assessment of bowel prep adequacy in outpatients. We aim to study the feasibility and acceptability of a VA in inpatients, and examine whether clinician assessment of pre-procedural bowel prep agrees with intra-procedural assessment.
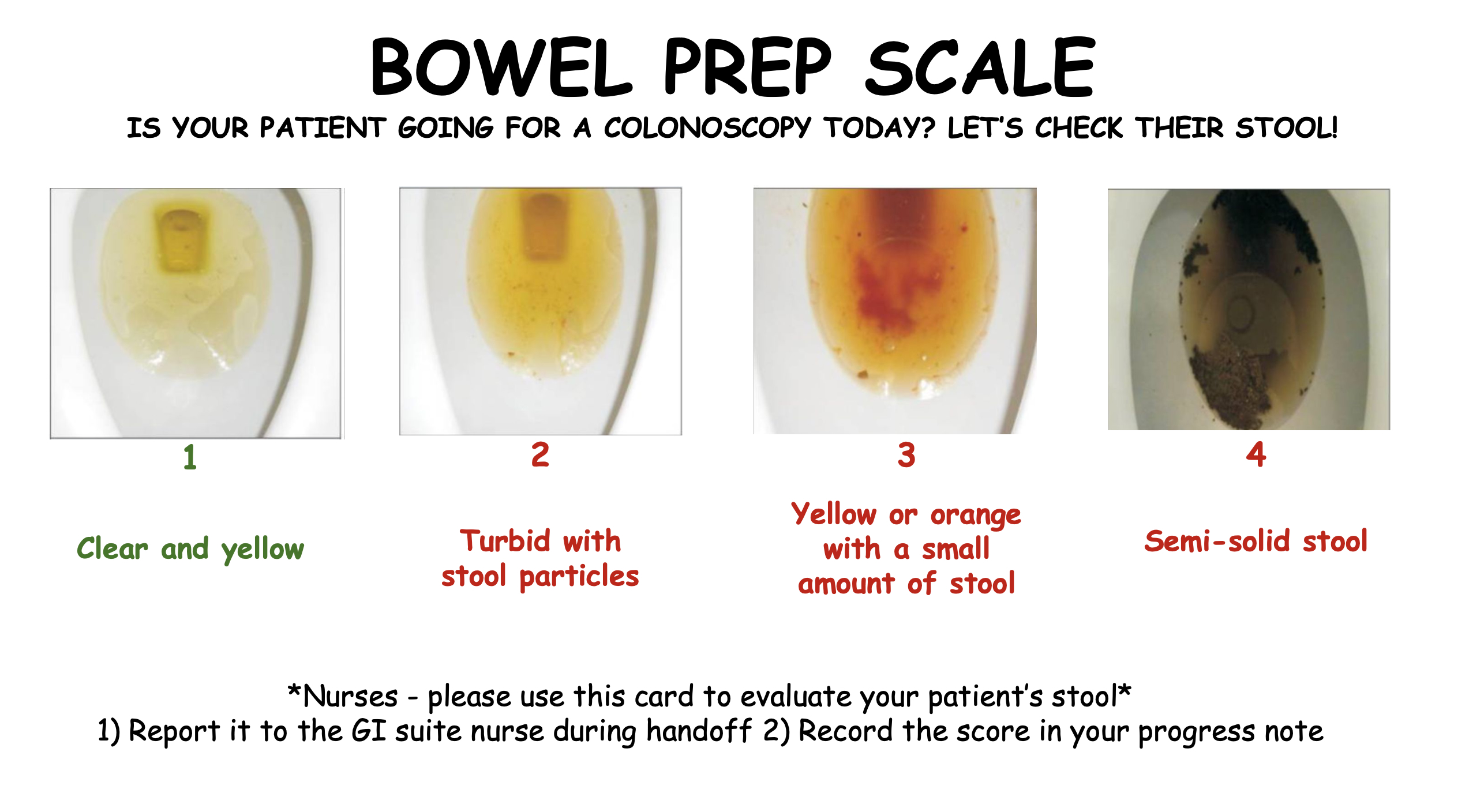
Methods: We conducted an IRB-approved single-center prospective pilot study from March-May 2024. We designed a VA using photos of four different bowel prep stages (So et al., 2015) each with a numerical score and description. Nurses were taught to use the VA to score bowel prep in their note and in handoff to the GI suite. Pre-procedural bowel prep adequacy was defined by a VA score of 1-2. Intra-procedural bowel prep adequacy (IP) was defined by Boston Bowel Preparation Scale (BBPS) > 6 and/or written assessment by the endoscopist (adequate for polyp > 6mm, “good”, “excellent”). Data were summarized via counts (%) and McNemar’s test was used to test disagreement. Preliminary nursing feedback on feasibility is in progress.
Results: 65 sequential inpatient colonoscopies were reviewed; 59 were ultimately included (Table 1). 50% of patients were female. Average age was 66 years old. The most frequent indication was iron deficiency anemia (IDA). 24 patients (41%) were successfully assessed using the VA. 16 (66%) patients had adequate bowel prep based on the VA, and 81% of these VA-assessed patients had adequate IP scores. Of the 8 patients with inadequate VA scores, 75% had inadequate IP scores. McNemar’s test did not show evidence of disagreement (p=0.65). In cases where the VA was not utilized, nurses described the stool in 57% of cases and blood was present in 11% of cases which impeded VA use.
Discussion: Although the VA was implemented in less than half of cases, we noted a strong trend in agreement between VA and IP scores. Both groups were similar except that patients not assessed by the VA were more often male and had more varied indications for inpatient colonoscopy, which warrant further investigation as potential barriers to VA implementation. We plan to expand our pilot study with regards to sample size, formal nursing feedback, and possible changes to the VA to better assess its utility in improving inpatient bowel prep.
So et al. Patient Descriptions of Rectal Effluents May Help to Predict the Quality of Bowel Preparation With Photographic Examples. Intest Res. 2015 Apr;13(2):153-9.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Anagha S. Nagaraj, MD1, Nicholas Costable, MD1, Shawneen Blaize, RN2, Emma Geraghty, RN2, Melissa Fazzari, PhD, MS1, Brett E. Fortune, MD, MS1, Harold Schwartz, MD1, Clara Y. Tow, MD1. P4082 - Will a Visual Aid Improve Colonoscopy Bowel Preparation in Hospitalized Patients? A Pilot Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY; 2Montefiore Medical Center, Bronx, NY
Introduction: Poor colonoscopy bowel preparation is a common and costly barrier to effective inpatient care. Prior studies have validated a visual aid (VA) as a tool for patient self-assessment of bowel prep adequacy in outpatients. We aim to study the feasibility and acceptability of a VA in inpatients, and examine whether clinician assessment of pre-procedural bowel prep agrees with intra-procedural assessment.
Methods: We conducted an IRB-approved single-center prospective pilot study from March-May 2024. We designed a VA using photos of four different bowel prep stages (So et al., 2015) each with a numerical score and description. Nurses were taught to use the VA to score bowel prep in their note and in handoff to the GI suite. Pre-procedural bowel prep adequacy was defined by a VA score of 1-2. Intra-procedural bowel prep adequacy (IP) was defined by Boston Bowel Preparation Scale (BBPS) > 6 and/or written assessment by the endoscopist (adequate for polyp > 6mm, “good”, “excellent”). Data were summarized via counts (%) and McNemar’s test was used to test disagreement. Preliminary nursing feedback on feasibility is in progress.
Results: 65 sequential inpatient colonoscopies were reviewed; 59 were ultimately included (Table 1). 50% of patients were female. Average age was 66 years old. The most frequent indication was iron deficiency anemia (IDA). 24 patients (41%) were successfully assessed using the VA. 16 (66%) patients had adequate bowel prep based on the VA, and 81% of these VA-assessed patients had adequate IP scores. Of the 8 patients with inadequate VA scores, 75% had inadequate IP scores. McNemar’s test did not show evidence of disagreement (p=0.65). In cases where the VA was not utilized, nurses described the stool in 57% of cases and blood was present in 11% of cases which impeded VA use.
Discussion: Although the VA was implemented in less than half of cases, we noted a strong trend in agreement between VA and IP scores. Both groups were similar except that patients not assessed by the VA were more often male and had more varied indications for inpatient colonoscopy, which warrant further investigation as potential barriers to VA implementation. We plan to expand our pilot study with regards to sample size, formal nursing feedback, and possible changes to the VA to better assess its utility in improving inpatient bowel prep.
So et al. Patient Descriptions of Rectal Effluents May Help to Predict the Quality of Bowel Preparation With Photographic Examples. Intest Res. 2015 Apr;13(2):153-9.
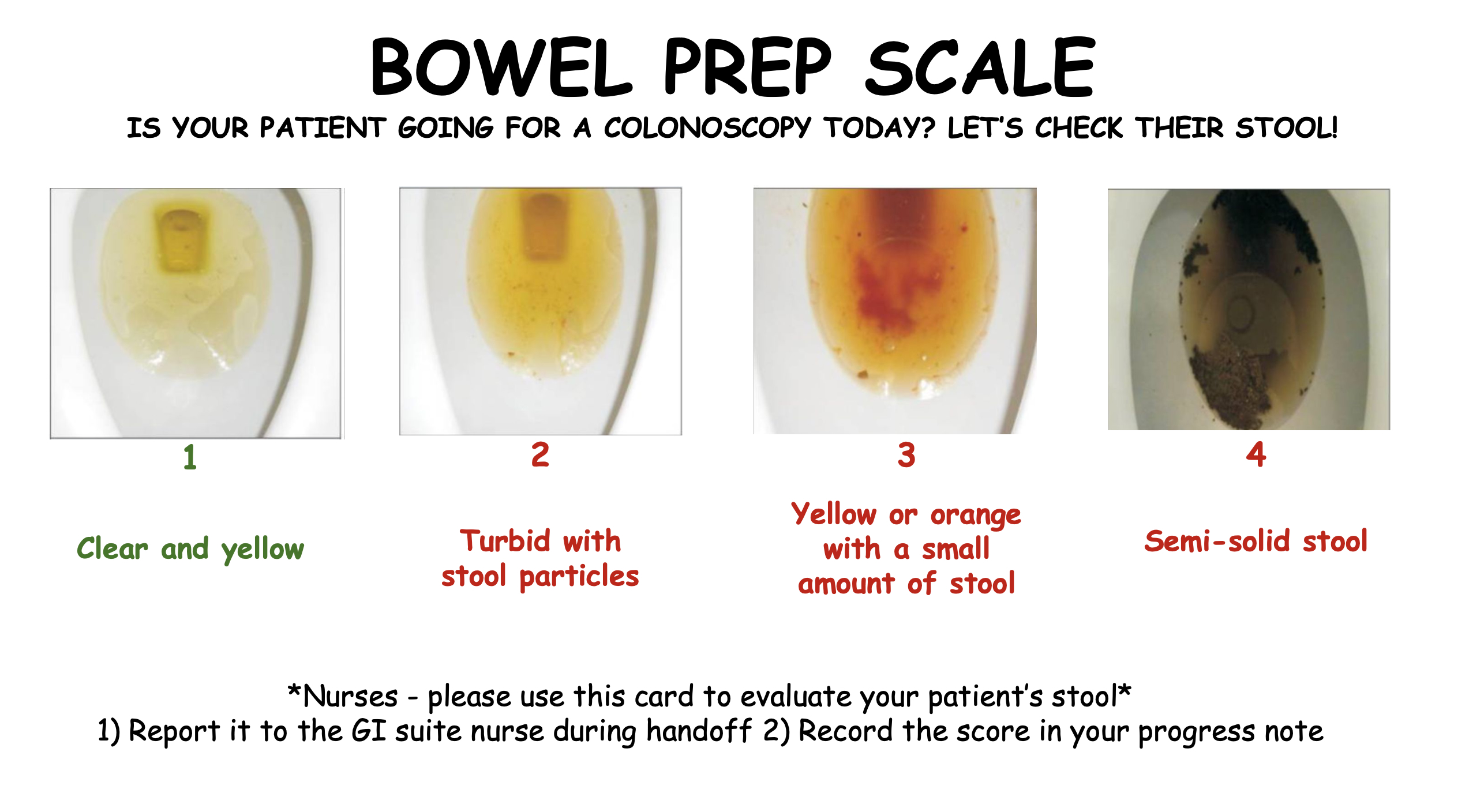
Figure: Visual Aid. Utilized by nurses to score bowel preparation adequacy prior to colonoscopy.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Anagha Nagaraj indicated no relevant financial relationships.
Nicholas Costable indicated no relevant financial relationships.
Shawneen Blaize indicated no relevant financial relationships.
Emma Geraghty indicated no relevant financial relationships.
Melissa Fazzari indicated no relevant financial relationships.
Brett Fortune: BD Medical – Consultant. Cook Medical – Consultant. WL Gore and Associates – Consultant.
Harold Schwartz indicated no relevant financial relationships.
Clara Tow indicated no relevant financial relationships.
Anagha S. Nagaraj, MD1, Nicholas Costable, MD1, Shawneen Blaize, RN2, Emma Geraghty, RN2, Melissa Fazzari, PhD, MS1, Brett E. Fortune, MD, MS1, Harold Schwartz, MD1, Clara Y. Tow, MD1. P4082 - Will a Visual Aid Improve Colonoscopy Bowel Preparation in Hospitalized Patients? A Pilot Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
